What is the best thing to eat while taking antibiotics? Nutrition during treatment with antibacterial drugs. Connection with food intake
Of all medicines, the highest effectiveness is observed with antibiotics. These drugs help cope with severe inflammatory processes, bacterial infections of various origins, and are prescribed as preventive measures during abdominal surgery, radiation and chemotherapy.
Before the invention of antibiotics, the mortality rate from bacterial infections was about 70%, and with the introduction of penicillin into circulation it decreased to 10-15%. However, potent substances can negatively affect health, so diet is important when taking antibiotics.
Why are antibiotics dangerous?
Any potent substance does not work locally, but has an effect on the entire body. An exception may be ointments and creams of superficial action, but if we are talking about injections or diffuse influences, then all systems receive a dose of medicine with the blood. The antibiotic diet takes into account the nuances of the effects of drugs on major organs, helping to prevent risks associated with side effects of medications.
Antibiotics are chemically enhanced toxins of certain types of molds. The first ones were made from the genus Penicillium, the newest ones also contain derivatives of the vital activity of the fungus in the form of toxic substances. Toxins destroy the shell of pathogenic bacteria, preventing “enemies” from multiplying in the human body. The principle of operation of these substances is also associated with risks: any antibiotic remains a highly toxic substance, so the load on the body must be reduced during administration. Considering that a person is already weakened by illness at the time of starting a course of potent medications, the diet should be maintained for several weeks. This implies a post-antibiotic diet.
What organs are harmed by antibiotics?
Medicines aimed at destroying bacterial infection have a complex effect. Therefore, it cannot be said that an antibiotic is only useful or only harmful - it is a medical procedure, but the treatment is aggressive. The patient should keep in mind that the drugs have a negative effect on the following organs and systems:
- Stomach - damage to the mucous membrane occurs, especially with oral, that is, in the form of tablets or capsules, use of medications.
- Liver - being a “station” for neutralizing toxic substances, the liver receives the greatest load, while simultaneously disposing of toxins from killed bacteria and antibiotics directly.
- Small intestine - absorption of food occurs in it, which occurs due to living symbiont bacteria. The antibiotic does not kill selectively; along with the “bad” microorganisms, the “good” ones also suffer.
- Large intestine - where food is finally divided into useful material and waste. Taking highly effective medicines also negatively affects beneficial microflora.
- Kidneys - along with the liver, perform a detoxification function, helping to cleanse the blood and remove toxic substances. Many antibiotics have a nephrotoxic effect, that is, they require special attention to the kidneys during administration and for several weeks after.
Diet during a course of antibiotics
There is no single menu that is universal for all cases when doctors prescribe potent drugs. Dietary guidelines and restrictions will depend on factors such as:
- The original disease is the reason for the use of antibiotics;
- Type of drugs;
- Method of administration - diffuse, injection, in the form of tablets;
- The patient’s health status, age, concomitant chronic diseases;
- Individual intolerances, allergies, food restrictions.
- Use the right products recommended as part of the course of treatment;
- Elimination of unhealthy foods, as well as those that are difficult to digest and absorb;
- The use of probiotics and prebiotics to regulate optimal microflora in the gastrointestinal tract;
- Correct drinking regime, aimed at detoxifying the body, removing residual substances and toxins.

Adhering to a diet in some cases is mandatory - for example, if the initial disease was associated with the gastrointestinal tract, and in others it is desirable, since it helps to avoid complications of both the disease itself and those associated with negative influence fungal derivatives on the human body.
How to eat during a course of antibiotics
Antibiotics are tolerated differently depending on the condition of the body. Children and the elderly perceive them worse, and during pregnancy, most types of these medications are contraindicated, except in cases that threaten the life of the mother. The average diet of an adult who does not have chronic diseases should be balanced and adhere to the following rules:
- Complete exclusion of alcohol. Ethyl-containing drinks neutralize the effect of medications. A significant increase in the load on the liver is fraught with nausea, vomiting, and systemic poisoning.
- It is not recommended to eat fried foods, which also have a harmful effect on the liver, stomach, small and large intestines. Fast food is completely avoided during intake and for five to six weeks after due to the high content of trans fats in such products.
- It is also necessary to exclude semi-finished products: canned food, sausage, smoked fish.
- It is important to remove salt from your diet or limit it as much as possible. This is done to facilitate the functioning of the kidneys.
- The drinking regime includes the mandatory consumption of two liters of clean still water per day. While taking antibiotics, it is advisable to reduce the amount of caffeine consumed in the form of strong tea and coffee. Energy drinks are not allowed.
Additional recommendations may include reducing spicy and hot foods, individual species vegetables and fruits - for example, cabbage, which is difficult to digest and puts a significant burden on the stomach. People with chronic diseases make up daily menu taking into account the basic requirements for your diet.
What to eat after a course of antibiotics
The diet after taking antibiotics for adults does not contain such serious restrictions as during treatment. It is only recommended to exclude alcohol, fast food and other obviously unhealthy foods. At the same time, there are specific features - recommendations for taking prebiotics and probiotics.
Prebiotics and probiotics are medications in the form of tablets, mixtures, or special products containing strains of beneficial bacteria. Since a course of aggressive treatment destroys those that inhabited the gastrointestinal tract, after completion of the course it is necessary to restore the population.
Do not take probiotics during a course of antibiotics! This is completely pointless: the medicine will kill them before the beneficial bacteria multiply.
Prebiotic drugs are sold in every pharmacy without a prescription. Despite this, many doctors advise repopulating your small and large intestines with proper nutrition. A diet for an adult that will help avoid dysbiosis and problems associated with this unpleasant condition includes:
- Kefir, yogurt and other fermented milk drinks. In supermarkets you can find branded products that specifically emphasize the increased content of beneficial bacteria. For the most part, this is an advertising gimmick - regular drinks based on sour milk will suffice.
- Symbiont bacteria feed on slow carbohydrates. An important part of the diet after antibiotics should be porridge made from unprocessed oats, bran, and brown rice.
- Fruits and vegetables rich in vitamins, such as tomatoes, bell peppers, apples, zucchini, pumpkin, onions and garlic if there are no contraindications, lemons, herbs, all types of berries.
- It is recommended to consume flaxseed.
- During the recovery period, products based on lean meat, poultry, and fish will be useful. It is advisable not to fry, but either steam it or use a slow cooker.

The disease weakens the body. Antibiotics, despite the fact that they help overcome the disease and get rid of infection, also tend to destroy the human body. Therefore, it is necessary to adhere to a diet that will help, on the one hand, cope with the disease, and on the other hand, spare and protect the main organs and systems. Remember that failure to comply with certain requirements, such as those regarding alcohol consumption, will negate the full benefit of medications.
The recovery period imposes fewer restrictions. Most of them relate to general ideas about proper nutrition and healthy image life. Wherein, main principle comes down to increasing the amount of probiotic agents that are aimed at restoring intestinal microflora. The second aspect involves strengthening the immune system and the body’s natural protective properties.
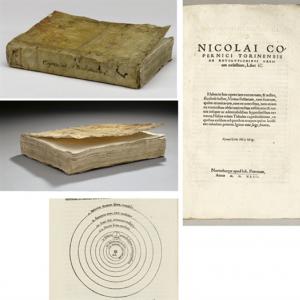
Back at the beginning of the 20th century, when Alexander Fleming discovered the world's first antibiotic, penicillin, he could not even imagine how great his discovery was. Indeed, the introduction of antibiotics was a real breakthrough in medicine. People stopped dying from infectious diseases; doctors could finally save a person from dysentery or typhoid.
But who would have thought that today, during modern technologies, the antibiotic should be taken according to certain rules. After all, this medicine can not only help. If the drug is not used correctly, the antibiotic can kill beneficial microorganisms along with harmful bacteria.
Do I need an antibiotic?
The most important rule is to take the antibiotic strictly as directed by the doctor. An antibiotic is a serious medicine, and you cannot decide to take it on your own. This drug group is prescribed only when the body is infected with pathogenic bacteria. Viral colds cannot be treated with antibiotics! There is no point in using an antibiotic for a runny nose, red throat (if there is no causative agent of streptococcus), or inflammation of the ear. All this can be treated symptomatically, plus you can take antiviral drugs.
However, other diseases cannot be cured without the use of antibiotics. They can manifest themselves as persistent, long-lasting and unbreakable temperatures, purulent discharge, infectious tissue lesions.
Only a doctor can determine the true need for antibiotics. Therefore, prescribing antibiotics yourself is extremely dangerous. In this case, the specialist must ask about the presence of allergic reactions to a particular drug, find out about previous experience of taking antibiotics, about chronic kidney or liver diseases, about the presence of diabetes mellitus. A woman must inform her doctor about a planned or current pregnancy, or about possible breastfeeding. All these nuances will help the doctor choose exactly the drug that will help get rid of the disease without leading to additional problems.
Some doctors may prescribe tests to determine the body's sensitivity to certain antibiotics. This will allow you to immediately choose a drug that is effective for you.
- When purchasing a medicine, pay attention to its expiration date - an expired medicine will not only be useless, it can be harmful. If the pharmacy does not have the medicine you specified, do not rush to replace it with an analogue - it is better to discuss this issue with your doctor.
- Typically, a prescription antibiotic should be taken two or three times a day. This means that the medicine must be taken at regular intervals. If you need to drink twice a day, then take it at 8 or 9 o’clock. In the morning and in the evening. If the prescription indicates three doses per day, then at 7, 15 and 23 hours. In this case, the effectiveness of the drug will be maximum.
- Some drugs need to be taken according to a specific schedule with varying amounts of the drug and time of administration. Please discuss this with your doctor.
- If you forget to take your medicine, take the missed dose as soon as you remember. Next appointment must be according to the scheme, without a time shift.
- The antibiotic should not be taken on an empty stomach. Due to the fact that this is a fairly aggressive medicine, it negatively affects the walls of an empty stomach. Take the medicine one hour after meals.
- If on the third day of taking antibiotics you notice an improvement in your condition, do not stop taking the drug. The fact is that antibiotics are a medicine that should be taken for at least five days, ideally 7 days. The fact is that in five days an antibiotic can completely suppress a harmful microorganism. And if you stop taking the medicine, the surviving bacteria can restore their population again and make a person sick.
- Very often the question arises about what form antibiotics should be prescribed. Of course, an antibiotic administered intramuscularly acts much faster and does not harm the walls of the stomach. This is especially true for patients with gastroenterological diseases. However, if we are talking about a child, it is better to take a suspension than to give an injection. For a child, a course of injections is incredibly stressful, which can only be justified by a real threat to his health.
- You need to take the medicine with warm water, never coffee, tea or sweet soda. This may cause allergic reaction body, and also lead to unexpected consequences.
- Antibiotics should never be mixed with alcohol. It is necessary to avoid taking alcoholic beverages during treatment. Alcohol-containing drinks can render the medicine completely useless. In other cases, alcohol taken with an antibiotic causes palpitations, tinnitus, and panic attacks.
- When taking medications of this group, it is important to follow some dietary rules. Eliminate acidic foods - fresh juices, vinegar, lemon.
- Some groups of antibiotics affect a person's tolerance to ultraviolet rays. Therefore, while taking these drugs, as well as for a couple of weeks after taking them, you should not sunbathe or visit a solarium.
These simple rules will make taking antibiotics comfortable and effective.
As the name suggests, an antibiotic kills living microorganisms. However, the disadvantage of this medication is that in addition to pathogenic bacteria, antibiotics also kill beneficial bacteria. This especially affects children and adults who are prone to gastroenterological diseases. Side effects such as constipation or diarrhea are common after taking antibiotics.

To restore healthy intestinal microflora, you need to immediately drink eubiotics along with the antibiotic. Linex, Bifidubakterin, Hilak Forte - all these medications will help you avoid intestinal upset after taking antibiotics. They need to be drunk according to the plan. They are usually taken 20-30 minutes before meals. This is an integral part of treatment when it comes to young children. In addition, you need to include natural bacteria in your diet - drink more fermented milk products. But do not take antibiotics with them - these medications do not tolerate being in the presence of lactic acid.
If you have liver problems, you probably feel a bitter taste in your mouth and nausea when taking antibiotics. To avoid this, you need to protect your liver during treatment. Take Gepatrim, Essentiale. In case of a serious illness, when taking antibiotics for a sufficiently long time, you can also take care of the prevention of fungal infections - for example, take Nystatin.
Antibiotics are the greatest invention of mankind. But only their correct use can be safe and effective. Take care of your health, follow your doctor's instructions and do not engage in amateur activities. And then your healthy body will be grateful to you.
Video: how to take antibiotics
The invention of antibiotics, which are well known to us, at one time made a real revolution in medicine. These drugs seemed magical; they made it possible to save the most critically ill patients with various pathologies of microbial origin. Unfortunately, in our time their capabilities have somewhat decreased. This is largely due to the too frequent prescription of antibacterial drugs and the increasing resistance of microbes to them. This is why it is so important to use all methods that help increase or maintain the effectiveness of antibiotics. One of them is proper nutrition.
If the doctor, for one reason or another, decides to prescribe you antibacterial agents, then you definitely need to clarify everything related to their use. AND proper diet plays far from being the least important (especially if medications must be swallowed and not administered through IVs or injections). Patients should be informed:
- on the impact of food components on the activity of pharmacological antibacterial drugs;
- about the influence of food intake on the effectiveness of antibiotics;
- about their incompatibility with certain products.
Let's consider some nuances of nutrition during the course of antibacterial treatment.
Food and antibiotic activity
While taking antibiotics, you need to monitor your diet, as some foods can weaken the effect of the medications.Once in our body, most antibiotics from digestive tract enters the blood, and then travels with it to the “targets” of its therapeutic effects. In case of absorption disorders or disturbances in the speed of passage through the gastrointestinal tube, the amount of active substances taken drug.
Thus, when eating excessively fatty foods (pork, lamb, curd mass, cakes with creams, etc.), refractory fats delay the residence of a number of antibacterial drugs in the stomach. There they are modified, which reduces their therapeutic activity. As a result, less drugs enter the intestine (where absorption occurs) than is necessary to destroy the infectious process. For this reason, when taking benzylpenicillins, lincomycin, biseptol, erythromycin, the fat quota in the diet should not be more than 40–50 g per day.
Optimal appointment time
Doctors do not talk about the connection between taking antibacterial agents and food just for the sake of formality. The food you eat affects the absorption of medications. So, if you take tetracycline in the middle of a hearty lunch, it will decrease by 50%. For this reason, all drugs in this group (with the exception of doxycycline) should be taken either an hour before meals or 3 hours after meals. The same rule applies to the group of penicillins, sulfonamides (cotrimoxazole, etc.), clindamycin, erythromycin, lincomycin.
But nitrofurans (furazolidone, etc.), isoniazid, metronidazole, nevigramon are advisable to take half an hour before the expected breakfast, dinner or lunch.
Food incompatibility
 The tablets should be taken only with water.
The tablets should be taken only with water. Many products contain substances that can block or significantly reduce the antimicrobial activity of antibiotics. Food with a high calcium quota (milk and its derivatives), even if taken at intervals of 10–15 minutes with tetracyclines (biomycin, oxytetracycline, doxycycline, etc.), reduces their therapeutic effect. In addition, milk is incompatible with ampicillin and reduces the therapeutic effect of nitrofurans due to its alkalizing effect.
Iron, aluminum and magnesium ions combine with antibiotic components to form insoluble chemical complexes. So when treating with polymyxin, clarithromycin, oleandomycin, it is better to reduce foods with big amount these minerals (meat by-products, beans, kelp, wheat bran, peas, dried fruits,).
In the case of prescribing sulfonamides (biseptol, etc.), it is recommended to beware of products with a large amount of benzoic acid and folic acid. They significantly reduce the therapeutic benefit of drugs and reduce their solubility, which leads to crystal deposition in the kidneys and urinary tract. And the crystals then gradually become stones. Such products include lingonberries, meat by-products, eggs, asparagus, cheese, spinach, nuts, beans, cabbage, etc.).
Most patients realize how dangerous it is to combine alcohol with antibiotics. The likelihood is growing side effects, the load on the already overworked liver increases, and other organs suffer. In addition, when treated with metronidazole and nitrofurans, alcohol often causes a disulfiram-like reaction in the form of severe nausea, facial flushing, vomiting, drop in blood pressure, increased heart rate, etc.). It is similar to the symptoms observed in “fixed” alcoholics who have violated the ban on strong drinks.
It is better to wash down any form of antibiotics (capsules, dragees, tablets) with plain boiled or still drinking water (50–100 ml is enough). Milk contains caseinogen, which upon contact with stomach juice is modified into calcium caseinate. This substance binds antibiotics tightly, reducing their absorption by 25–80%.
How to neutralize the unwanted effects of antibiotics with food
Antibiotics can aggravate existing problems, as they affect certain areas of metabolism. Tetracyclines increase the risk of or worsen deficiency ascorbic acid. Isoniazid, prescribed for tuberculosis, neutralizes the effects of vitamin B6, and streptomycin – vitamin B1. Therefore, during antibiotic therapy, the content of these substances in the diet should be normal or even slightly higher.
Strict vegetarianism is also extremely undesirable, since treatment with aminoglycosides (gentamicin, etc.) in those who oppose meat increases the likelihood of hypovitaminosis B12 and all the effects of caffeine are enhanced. And with therapy with nitrofurans (furazolidone, etc.), the risk of neurological disorders increases.
Educational video on the topic “Why antibiotics don’t always work”:
It’s hard to imagine, but back at the beginning of the 20th century, thousands of people died from various infectious diseases - pneumonia, typhoid, dysentery. And only with the advent of antibiotics did all these terrible diseases recede. Today, a doctor has several groups of antibiotics in his arsenal, different in their direction of action - antibacterial, antifungal, antitumor.
Antibiotics are also different in origin - they are natural, semi-synthetic and synthetic drugs. Natural antibiotics are made from fungi or bacteria, and the largest group, including 80% of all drugs, are drugs obtained from actinomycetes (, streptomycin, erythromycin). Semi-synthetic antibiotics are products of modification of natural molecules (cefazolin, amoxicillin, etc.). The group of synthetic antibacterial drugs includes quinolones, nitrofurans, sulfonamides, etc. There are also groups of antibiotics of animal and plant origin.
The mechanism of action of the antibiotic is that it either inhibits the growth of microbes (cytostatic effect), or kills cells (cytocidal), or dissolves the cell membrane, which also leads to cell death (cytolytic) of the bacteria. The spectrum of bacterial action is determined by the types of microorganisms that are sensitive to a particular drug. Narrow-spectrum antibiotics act predominantly on gram-positive microorganisms () or predominantly on gram-negative microorganisms (polymyxins). Broad-spectrum antibiotics include aminoglycosides, tetracyclines, and 3rd generation cephalosporins.
Strictly as prescribed by the doctor
Antibiotic drugs are successfully used in the treatment of many diseases: sinusitis, pneumonia, bacterial infections gastrointestinal tract, infections of the genitourinary system, sexually transmitted infections, purulent inflammations of the skin, etc. They are effective in cases where bacteria are the cause of the disease. But they are absolutely useless for diseases caused by viral infection, such as ARVI, tracheitis, bronchitis, pharyngitis. Although sometimes bronchitis can be caused by a mixed infection - viral and bacterial.
In any case, the treatment tactics must be determined by the doctor. Only a doctor can distinguish a bacterial infection from a viral one and correctly select the necessary medications. Self-medication, even with a trivial one, is undesirable. After all, each antibiotic acts strictly on a specific group of microorganisms that are sensitive to it. The wrong choice of drug, dosage, and duration of use are fraught with negative health consequences, for example, suppression of natural microflora, weakened immunity, and the development of chronic diseases. Using antibiotics for insurance or for prophylactic purposes is also unacceptable.
With important additions
In order to prescribe adequate treatment and prescribe the necessary medication, the doctor must have not only information about the symptoms of the disease. Therefore, it is important for the patient to answer clarifying questions:
Have you ever experienced any side effects while taking medications?
Are you allergic to any medications?
Do you suffer from serious liver, kidney, stomach or diabetes mellitus?
Are you currently taking other medications?
A woman must report pregnancy (or planned pregnancy), and also whether she is a nursing mother.
These are very important details that allow you to select medications as accurately as possible and determine the required doses, taking into account the patient’s current health condition and the presence of concomitant diseases. For example, many antibiotics are incompatible with antacid drugs that are prescribed for stomach diseases. If these medications need to be taken at the same time, your doctor will determine the optimal dosage and timing to get the most from your treatment.
Following the rules
The action of antibacterial drugs will be effective when creating the required concentration of the drug in the body. To accomplish this task, there are certain rules for taking antibiotics that are important to follow.
Antibiotics must be taken strictly according to the regimen prescribed by the doctor and in accordance with his recommendations.
The drug is taken as many times a day as prescribed by the doctor. If it is indicated - 3 times a day, this means that the medicine must be taken at equal intervals, after 8 hours: at 8 o'clock, 16 o'clock and 24 o'clock. The instructions attached to each drug also indicate the method of use and dosage.
It is necessary to strictly adhere to the time of taking the antibiotic, but if for some reason the schedule was disrupted, you need to take the drug as soon as possible.
You cannot independently increase or decrease the dosage recommended by your doctor. The dose of the drug is calculated individually for each patient, taking into account his age and the presence of concomitant diseases.
If the pharmacy does not have the required drug and the pharmacist suggests replacing it with an analogue, it is advisable to coordinate this issue with your doctor.
Take antibiotics with water room temperature. You should not use tea or coffee, they accelerate the elimination of the drug, reducing the effectiveness of treatment. It is also not recommended to take medications with juices. Juices contain phosphoric acid, which can react with the components of the drug and cause poisoning.
Don't forget the details
The effectiveness of antibiotic therapy also depends on other, seemingly insignificant, factors that are usually ignored by many patients. Therefore, during treatment you need:
Adjust your diet and avoid foods with increased content acids (sour fruits, juices, drinks, dishes prepared with vinegar).
It is advisable to exclude alcoholic drinks. Under the influence of alcohol, the effect of antibiotics weakens, the components of the drug lose their activity, accumulate in the body and poison it. Or, on the contrary, they increase the effect many times over, which can lead to unpredictable consequences. Some drugs (tinidazole, furazolidone, cotrimoxazole, etc.) are strictly not recommended to be combined with alcohol. This is also stated in the instructions for use.
Do not use expired antibiotics. They have a toxic effect on the body and increase the likelihood of side effects.
Avoid sunbathing or visiting a solarium while taking antibiotics, as well as for two weeks after the end of treatment. Most antibiotics, such as quinolones, increase skin sensitivity to ultraviolet rays.