Legs run at night. Causes and treatment of restless legs syndrome at home. Restless legs syndrome causes
The human body is capable of coping with stress on its own. If there is a lot of tension in your body, if you are nervous or constantly tired, you may sometimes notice involuntary twitching or movements of your legs. This is how relaxation happens. However, if you notice this regularly, and not as an isolated case, if in a relaxed state your legs are still tense and do not obey, it is better to consult a specialist. It could be RLS - restless legs disease.
The first symptom of restless legs is that there is discomfort in the legs in the evening or at night. It is worth considering environment(fatigue, heels), but you shouldn’t wait months or years. The sooner you start treatment, the faster the results will appear. Self-medication can help initial stage, but the probability is still lower than if you contact a specialist. The effect of massage, rubbing and warming the feet is often very short-lived and at the same time misleading and delays your trip to the doctor.
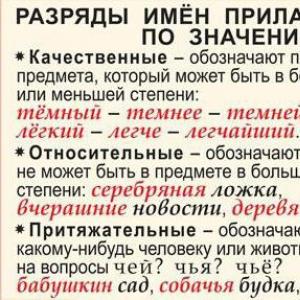
At the same time, if a doctor had immediately told us how to treat this condition in case of restless legs syndrome, many would have long lived a full life without suffering. The disease has its own characteristics, knowing which you can quickly identify it. With restless legs syndrome, the symptoms are usually the following:
- Discomfort. This includes aching pain and even its absence. What is usually felt is “pins and needles”, a tingling and pressure sensation, and itching that is quite severe or prolonged. These conditions are observed in the legs, but can also appear higher, up to the arms.
- Evening and night time. The hardest time for RLS sufferers is from midnight to 4 a.m., after which the symptoms subside. Interestingly, this cannot be confused with overwork: RLS manifests itself even without overwork during the day. There will be no symptoms during the day, even during sports or other activities.
- Leg movements at rest. As mentioned at the beginning, the brain will try to remove the discomfort and tell the muscles to relieve tension. They will begin to twitch. sway or even contract convulsively, and all this while the legs are at rest. If you get up and walk around, the symptoms will almost disappear. But they will return at the next relaxation.
- Lack of control. This is the most unpleasant symptom. A person even with a stronger will cannot influence RLS. And even the more he relaxes, the more he can manifest himself. And since the legs move most often at night, sleep problems may begin.
- Ineffective self-medication. Folk and home methods for RLS do not help or lead only to short-term changes in the condition. And when complications arise, symptoms sometimes appear during the day.
Causes of restless legs
In pregnant women, restless legs syndrome occurs in 20% of cases, and it can intensify due to toxicosis. But there is good news: if RLS is caused only by pregnancy, then a few months after the birth of the child, the symptoms will disappear without a trace.
The peculiarity of RLS is that it can be both congenital (primary type) and acquired (secondary type). The first can appear in a completely healthy person for no reason; it is often determined genetically and is inherited. If this is the first type, then the first symptoms may appear already in childhood or adolescence.
But the secondary one develops, as a rule, in older people. It has its own prerequisites, these include chronic diseases. It can be caused by negative changes in the functioning of such areas of health as:
- endocrinology: interruptions in the thyroid gland and pituitary gland, the presence of diabetes mellitus;
- neurology: symptoms develop in the presence of polyneuropathy, fibromyalgia, Parkinson's disease, essential tremor, multiple sclerosis;
- circulation: RLS may be caused by thrombosis lower limbs, vascular sclerosis, arterial diseases.
The syndrome can also appear when:
- infectious and non-infectious arthritis and arthrosis;
- oxygen deficiency due to chronic lung diseases;
- diseases of the spine or malfunctions of the spinal cord, injuries;
- neoplasms and inflammation in the brain;
- genetic and autoimmune diseases.
In pregnant women, restless legs syndrome occurs in 20% of cases, and it can intensify due to toxicosis. But there is good news: if RLS is caused only by pregnancy, then a few months after the birth of the child, the symptoms will disappear without a trace.
What gives a severe form of the disease is alcoholism, drug addiction and even caffeine abuse. This happens because the central nervous system is stimulated more than necessary, and the brain sends the wrong signals to the muscles. Success in treatment here largely depends on the transition to healthy image life.

How is RLS diagnosed?
Taking into account the causes of restless legs syndrome, treatment will be prescribed after consultation with relevant specialists: endocrinologist, neurologist, etc. First, the doctor will determine the type of disease (primary or secondary), then check for hormonal imbalances and, if necessary, prescribe several more consultations. Most likely you will need:
- go to an appointment with a neurologist;
- take blood tests (general, detailed, hormone levels and iron levels).
There are also less common methods for detecting the disease, but they are sometimes used. These include:
- electromyography and electroencephalogram. During the procedure, using special devices, the doctor will be able to measure your muscle activity and brain characteristics;
- computed tomography or magnetic resonance imaging. It is necessary when the presence of neoplasms is possible.
- somnography. This analysis makes it possible to understand whether the onset of the disease is associated with sleep problems, as well as which of the problems was primary.
But what to do with restless legs syndrome, which manifests itself along with a chronic disease, being secondary? The main thing is to remain calm and go for a consultation with the right doctor: an endocrinologist, cardiologist, etc. There are cases when this problem is genetic. Then you need to contact a geneticist, and he will conduct research, find out the reasons and select individual appropriate drugs and procedures. And if your legs are burning, treatment is simply necessary.
Treatment of RLS using traditional methods
Treatment of restless legs syndrome with traditional methods is most often symptomatic. If it turns out that the disease is of the primary type, then it will be difficult to fight it, only to alleviate the condition. Stable long-term remission or a significant delay in the development of the disease may occur. For this purpose they prescribe:
- sedatives to help you relax and sleep better;
- drugs against seizures if there are strong muscle contractions that cannot be controlled;
- dophamergics - medications that produce more dopamine;
- pain medications – used only for a short period of time;
- physiotherapy: massage various types, oxygen and other therapeutic baths, various wraps with therapeutic mud, as well as myostimulation.
If you approach the treatment of restless legs in a comprehensive manner, you can get a good result in 1-2 weeks. Unfortunately, if the form of the disease is primary, then alleviating the condition is all that can be done. It is proposed to use folk remedies and carry out prevention.
In the case where the type is secondary, they initially fight the underlying disease. All of the above are also prescribed, but only as complex therapy, and more attention is directed to eliminating the cause, rather than the symptoms.
Treatment of RLS with folk remedies
If restless legs syndrome is detected, treatment folk remedies may be fraught with difficulties. The reason for this is the possibility of allergies, as well as individual intolerance and pregnancy. Nevertheless, traditional methods You can use them, but they need to be selected correctly, taking into account all contraindications. The result will only come with responsible and long-term use.
This treatment of restless legs syndrome, as a combination of traditional methods and preventive procedures, is optimal comprehensive solution Problems. Typically the following rules must be followed:


Folk remedies differ from traditional ones in that they take a little longer for you to notice the results. But over time, they will prove their effectiveness and help eliminate restless leg syndrome. If you choose massage and herbs, then do these procedures for about 2-3 weeks, no less. And if the disease is no longer at the very initial stage, then the period can be increased to 2 months. Remember: if the result is minimal, or even after 2 months the condition does not improve, be sure to consult a doctor to avoid complications.
Currently, many are interested in what restless legs syndrome is, causes and treatment. We will find out who most often suffers from this disease, get acquainted with the symptoms of restless limbs, and find out what to do to improve the quality of sleep.
.jpg" alt="restless legs syndrome causes and treatment" width="500" height="261" srcset="" data-srcset="https://i0.wp..jpg?w=500&ssl=1 500w, https://i0.wp..jpg?resize=300%2C157&ssl=1 300w" sizes="(max-width: 500px) 100vw, 500px" data-recalc-dims="1">!} 
It is important to know what traditional and folk methods of treating tired legs syndrome exist in order to get rid of the irresistible desire to move your legs incessantly.
General information about the disease
Humanity has been familiar with this disease for a long time. Information about it first appeared in 1672, described by Thomas Willis, and was explored more deeply by the Swede Ekbom in the mid-20th century. Therefore, restless legs syndrome (RLS) is called by their names: Willis disease, Ekbom disease.
The disease is characterized by extremely uncomfortable sensations in the legs. They appear in the evening before bed, disappear in the morning and do not bother you in the first half of the day. Tired leg syndrome is one of the causes of insomnia.
Restless limb syndrome can also occur during daytime sleep, when you just lay down to rest. A person experiences suffering without pain- This is a distinctive feature of the RLS.
.jpg" alt="General information about the disease, Willis syndrome" width="500" height="251" srcset="" data-srcset="https://i2.wp..jpg?w=500&ssl=1 500w, https://i2.wp..jpg?resize=300%2C151&ssl=1 300w" sizes="(max-width: 500px) 100vw, 500px" data-recalc-dims="1">!}
This disease is detected in 10% of the world's population. It is more often found in older people (35-70 years). The female population suffers from RLS more often. Can also be diagnosed in children. This is often associated with the child's hyperactivity and lack of attention. This is only a hypothesis, not confirmed by anything.
Restless legs syndrome causes and treatment: classification of the disease
According to its genesis, restless legs syndrome causes and treatment are divided into 2 groups:
- idiopathic syndrome (primary)
- symptomatic syndrome (secondary)
Primary syndrome – little studied, young people under 30 years of age are affected. Not associated with major diseases, it accounts for up to 50%. Accompanies a person throughout his life, alternating periods of progression and remission. Occurs suddenly, the reasons are not clear, it may be:
- heredity in 20-70% of cases
- disturbances in the functioning of the central nervous system
- psychological circumstances (stress, depression, fatigue)
Secondary syndrome– manifests itself against the background of an underlying (neurological or somatic) disease, disappears after their elimination. Frequently encountered:
- anemia due to iron deficiency
- diabetes, thyroid diseases
- abuse of alcohol, tobacco, caffeine
- interruption in blood supply
- kidney diseases, arthritis
- vitamin deficiency (group B) and magnesium deficiency
- treatment with certain medications
Secondary syndrome occurs after 40 years of age or later. The exception is pregnancy. More than 16% of pregnant women suffer from this disease, 3 times more than non-pregnant women. There is a possibility of genetic transmission of RLS from mother to fetus, which poses a threat to pregnancy.
If you ever woke up with cramps in your arms or legs, then you have experienced the symptoms of restless leg syndrome. The disorder is mainly characterized by sudden or unpredictable spasms or jerking of body limbs. Although it primarily occurs in the legs, as the name suggests, the syndrome can also affect the torso, head, and arms.
Restless legs syndrome is considered a serious problem as the severity of its symptoms can range quite dramatically, ranging from mild irritation to constant sleep disruptions and severe impact on quality of life. Limb twitching is actually a secondary symptom, as most people who suffer from this syndrome complain of itching, muscle pain, electrical impulses, or even the sensation of something crawling on their body.
.jpg" alt="The most common symptoms of restless legs" width="500" height="283" srcset="" data-srcset="https://i0.wp..jpg?w=500&ssl=1 500w, https://i0.wp..jpg?resize=300%2C170&ssl=1 300w" sizes="(max-width: 500px) 100vw, 500px" data-recalc-dims="1">!} 
Cramps most often occur at rest, which often precedes sleep, or when the body is relaxed and motionless. There are many causes of this syndrome, but the most common explanation is iron deficiency. So, if you have iron deficiency or excess, your chances of developing this syndrome increase significantly.
Restless legs syndrome can be accompanied by other health problems such as sleep apnea, thyroid disease, Parkinson's disease, and magnesium deficiency.
There are some symptoms that will help you determine if you have restless leg syndrome yourself. Forums are full of recommendations and reviews on how to diagnose Willis disease. The presence of these symptoms does not negate a trip to the doctor:
- convulsions, sensitivity disorders, unbearable itching, goosebumps
- most often, unpleasant sensations occur in both legs, mainly the lower leg is affected
- there is an unbearable need to move your legs, there may be involuntary movements
- symptoms intensify in the evening, become simply unbearable at night, and weaken by morning
- cyclical movements of the lower extremities during sleep
- Symptoms increase with age, insomnia
Very often a person cannot find the right word to describe the symptoms. In the summer, these symptoms worsen. There is a hypothesis that this is due to excessive sweating. Another oddity is that the more physical activity, the less noticeable the symptoms.
Diagnostic criteria for Willis disease
Diagnostic criteria have been developed for staging DS restless lower limb syndrome, which are based on objective complaints from patients:
- irresistible desire to move limbs
- painful sensations occur at rest with a gradual increase
- with active movement they decrease or disappear
- unpleasant effects are aggravated in the evening and at night and during sleep
These signs are universal, and if the answer is yes, a positive diagnosis can be made. In addition, a laboratory examination is carried out to identify the underlying disease.
Complex therapy for restless legs syndrome
A specific algorithm for the treatment of restless legs syndrome has been developed, which includes a number of procedures. This includes:
- drug therapy
- physical therapy and physiotherapy
- help from a psychotherapist
- folk remedies and homeopathy
- self help, bedtime ceremony
Once the diagnosis is made, comprehensive treatment of Ekbom's disease can begin. Drug therapy depends on whether it is a primary or secondary syndrome.
Treatment of primary syndrome
With primary RLS, symptomatic treatment predominates, as a result of which it is possible to significantly alleviate the condition. It includes non-drug and drug therapy. At this stage it is important to cancel and not prescribe medicines, increasing the manifestations of RLS.
It is necessary to eliminate the lack of iron in the body (namely, in the brain), normalize blood glucose, replenish the deficiency of vitamins and magnesium, and use it for this purpose.
.jpg" alt="Magne B6" width="300" height="300" srcset="" data-srcset="https://i2.wp..jpg?resize=500%2C500&ssl=1 500w, https://i2.wp..jpg?resize=150%2C150&ssl=1 150w, https://i2.wp..jpg?resize=300%2C300&ssl=1 300w" sizes="(max-width: 300px) 100vw, 300px" data-recalc-dims="1">!}
The prescription of dopaminergic drugs (Nakom, Bromocriptine, Mirapex) is of great importance.
.big_.jpg" alt="Mirapex for restless leg syndrome" width="400" height="400" srcset="" data-srcset="https://i2.wp..big_.jpg?w=400&ssl=1 400w, https://i2.wp..big_.jpg?resize=150%2C150&ssl=1 150w, https://i2.wp..big_.jpg?resize=300%2C300&ssl=1 300w" sizes="(max-width: 400px) 100vw, 400px" data-recalc-dims="1">!}
Mirapex is taken ½ tablet at night, relief is often observed within an hour. Drugs that affect sleep (Clonazepam, Alprazolam) and anticolvunsants (Carbamazepine, Gabapentin) are prescribed.
The disadvantage of treatment is that it can last for years. You may become accustomed to the drug and will have to replace it. One should strive to use medications in very small dosages.
Non-drug therapy includes giving up bad habits (alcohol, tobacco, caffeine), evening walks fresh air, adequate inactive physical activity, physiotherapy (magnet, mud). Acupuncture, massage, electrical stimulation and cryotherapy provide a good therapeutic effect.
With a moderate load on the legs during the day, squats, stretching the calf muscles. Gentle running, cycling, walking, tiptoeing. Leg extension and bending exercises.
.jpg" alt="Therapeutic exercise" width="500" height="496" srcset="" data-srcset="https://i2.wp..jpg?w=500&ssl=1 500w, https://i2.wp..jpg?resize=150%2C150&ssl=1 150w, https://i2.wp..jpg?resize=300%2C298&ssl=1 300w" sizes="(max-width: 500px) 100vw, 500px" data-recalc-dims="1">!}
Treatment of secondary syndrome
With secondary RLS, treatment of the underlying disease is required. And only after the underlying disease that provokes restlessness in the limbs has been cured, therapy for the syndrome can begin.
Subsequent therapy is the same as for the primary syndrome.
Fatigue limb syndrome can be successfully treated with properly selected therapy.
Therapy with folk remedies, homeopathy
Let's consider what traditional healers and homeopaths advise for such a disease. After all, if you can do without synthetic products and not strain your liver once again, then why not try them first.
ethnoscience
Traditional medicine also did not stand aside from the treatment of restless legs syndrome and offered its own methods for relieving the painful effects. Here are some of them:
Data-lazy-type="image" data-src="https://prozdorovechko.ru/wp-content/uploads/2017/01/nogi1.jpg" alt=" Therapy with folk remedies, homeopathy" width="500" height="294" srcset="" data-srcset="https://i0.wp..jpg?w=500&ssl=1 500w, https://i0.wp..jpg?resize=300%2C176&ssl=1 300w" sizes="(max-width: 500px) 100vw, 500px" data-recalc-dims="1">!}
All these simple measures will help reduce or completely get rid of unpleasant symptoms, and it will be possible to return to normal living conditions.
What to take from homeopathy
Since with mono-preparations a complex individual selection of a professional homeopath is important (such training is available in England), it is better to use ready-made complexes developed by professionals, which can be found in homeopathic pharmacies or the iHerb online store.
Data-lazy-type="image" data-src="https://prozdorovechko.ru/wp-content/uploads/2017/01/homeopathy1.jpg" alt="Hyland"s, Restful Legs " width="300" height="301" srcset="" data-srcset="https://i0.wp..jpg?w=500&ssl=1 500w, https://i0.wp..jpg?resize=150%2C150&ssl=1 150w, https://i0.wp..jpg?resize=300%2C300&ssl=1 300w" sizes="(max-width: 300px) 100vw, 300px" data-recalc-dims="1">!}
For those who live in large cities where there are homeopathic pharmacies, here is a list of ready-made homeopathic complexes for tired legs syndrome:
data-lazy-type="image" data-src="https://prozdorovechko.ru/wp-content/uploads/2017/01/homeopathy.png" alt="list of ready-made homeopathic complexes for tiredness syndrome legs" width="640" height="394" srcset="" data-srcset="https://i2.wp..png?w=731&ssl=1 731w, https://i2.wp..png?resize=300%2C185&ssl=1 300w" sizes="(max-width: 640px) 100vw, 640px" data-recalc-dims="1">!}  Now you have the opportunity to choose where to start treating your restless legs. Be sure to consult with your doctor when choosing treatment to ensure it is most effective.
Now you have the opportunity to choose where to start treating your restless legs. Be sure to consult with your doctor when choosing treatment to ensure it is most effective.
How to help yourself at home - 9 tips
In the evening before going to bed, carry out distracting activities: take a walk in the air, have a drink Herb tea with valerian, take a warm shower.
It is necessary to develop a ceremony for going to bed, make contrasting baths with hot and cold water. We need to finish them hot water, then rub well with a towel and cover with a warm blanket. Sleep on your side with a pillow between your knees.
Elena Malysheva gives the same advice in her program:
This is also true for pregnant women, as blood circulation improves and discomfort goes away.
If, nevertheless, the attack could not be avoided, you can sit on the bed and rub your legs well or massage them. It is not recommended to get up, otherwise sleep will disappear completely.
While many doctors recommend a variety of medications, ranging from antiemetics and antidepressants to anticonvulsants, there are also many natural ways to relieve the symptoms of this syndrome yourself at home. We'll talk about this later.
1. Sex
Data-lazy-type="image" data-src="https://prozdorovechko.ru/wp-content/uploads/2017/01/1.jpg" alt="How to help yourself at home - 9 tips" width="300" height="209" data-recalc-dims="1">!}  One of the simplest and most enjoyable ways to cure the syndrome is regular sex.
One of the simplest and most enjoyable ways to cure the syndrome is regular sex.
The strong release of endorphins and the subsequent period of relaxation that follows sexual intercourse are associated with lower rates of RLS symptoms.
Therefore, do not deny yourself this pleasure.
Jpg" alt="Reduced caffeine" width="300" height="234" data-recalc-dims="1">!}  As everyone knows, caffeine is known as an energy booster (especially in the morning), but it is also a strong stimulant. If you consume high levels of caffeine, your body may remain overstimulated throughout the day as well as at night.
As everyone knows, caffeine is known as an energy booster (especially in the morning), but it is also a strong stimulant. If you consume high levels of caffeine, your body may remain overstimulated throughout the day as well as at night.
Stimulants affect the nervous system, which is the main system associated with restless leg syndrome. If you suffer from the syndrome, one of the first ways to stop symptoms is to avoid coffee in the afternoon.
Jpg" alt="Massage" width="300" height="142" data-recalc-dims="1">!}  Relaxation massage is an excellent way to alleviate or eliminate the symptoms of this syndrome. Not only does this help release toxins and ease muscle pain, but you will also be able to calm down and relax.
Relaxation massage is an excellent way to alleviate or eliminate the symptoms of this syndrome. Not only does this help release toxins and ease muscle pain, but you will also be able to calm down and relax.
Chronic stress and muscle tension can lead to RLS, and one of the the best ways defeat stress - feel great, and for this you should visit a massage at least a couple of times a month.
4. Tea
Data-lazy-type="image" data-src="https://prozdorovechko.ru/wp-content/uploads/2017/01/45647690.jpg" alt="Green tea" width="300" height="170" data-recalc-dims="1">!}  Teas from all varieties contain soothing and beneficial compounds, including catechins, vitamins, polyphenols, flavonoids and other anti-inflammatory substances.
Teas from all varieties contain soothing and beneficial compounds, including catechins, vitamins, polyphenols, flavonoids and other anti-inflammatory substances.
The tea helps calm our mind and body and is highly recommended for people suffering from RLS. Green and chamomile teas work best and are also excellent substitutes for coffee - they also contain caffeine, but in smaller quantities.
5. Valerian
Data-lazy-type="image" data-src="https://prozdorovechko.ru/wp-content/uploads/2017/01/valeriana_korni.jpg" alt="Valerian root" width="300" height="247" data-recalc-dims="1">!}  Valerian root is a very popular remedy and is widely known for its ability to relax muscles and improve sleep.
Valerian root is a very popular remedy and is widely known for its ability to relax muscles and improve sleep.
Essentially, valerian can “kill two birds with one stone” - it not only soothes muscles, eliminating spasms and tremors, but also promotes deep sleep.
As a result, the body is in a state of complete rest, and the symptoms subside.
Jpg" alt="Regular walks" width="300" height="200" data-recalc-dims="1">!}  Normal blood flow is important for overall health, but is also key to treating RLS.
Normal blood flow is important for overall health, but is also key to treating RLS.
With normal blood circulation, our metabolism also works at normal level, as a result, almost all body processes improve, including the absorption of iron in the intestines and work nervous system, which prevents tremors and cramps at night.
As you know, regular walks have a very good effect on our blood circulation.
0.jpg" alt="Regular stretching" width="300" height="201" data-recalc-dims="1">!}  Stretching is key to healthy muscles, and it not only prevents injury, but also reduces the occurrence of RLS.
Stretching is key to healthy muscles, and it not only prevents injury, but also reduces the occurrence of RLS.
This is especially helpful if you do stretching before and after physical exercise, and also before bedtime.
This will help get rid of the symptoms of Willis disease and make you sleep soundly.
Jpg" alt="Wear socks" width="300" height="189" data-recalc-dims="1">!}  Although this is not clear to science, there is anecdotal information from people who suffer from this syndrome.
Although this is not clear to science, there is anecdotal information from people who suffer from this syndrome.
They claim that wearing socks helps reduce symptoms.
This may be due to the numerous nerve endings in the feet that are more easily stimulated by walking barefoot.
Jpg" alt="Change your diet" width="300" height="158" srcset="" data-srcset="https://i0.wp..jpg?w=634&ssl=1 634w, https://i0.wp..jpg?resize=300%2C158&ssl=1 300w" sizes="(max-width: 300px) 100vw, 300px" data-recalc-dims="1">!}  Your diet can have a significant impact on your nervous system, as well as every organ and system in the body. Depending on the reason for your syndrome (iron deficiency, magnesium deficiency, diabetes, etc.), it is worth changing your diet accordingly.
Your diet can have a significant impact on your nervous system, as well as every organ and system in the body. Depending on the reason for your syndrome (iron deficiency, magnesium deficiency, diabetes, etc.), it is worth changing your diet accordingly.
Increasing your iron intake is easy—just add red meat, beans, spinach, and grains to your diet. First go to the doctor and consult with him, and then you can make the necessary adjustments to your diet.
Bottom line: 9 tips on how to get rid of tired leg syndrome at home are very simple and anyone can do them.
Preventing restless leg syndrome
Prevention measures are simple and easy for anyone to implement. Don’t forget to do morning exercises, walking, alternating work and rest. Intellectual challenges are welcome. Eliminate stress loads.
Consult your doctor and, if possible, stop the following medications that may cause restless legs syndrome, especially if you are predisposed to it:
data-lazy-type="image" data-src="https://prozdorovechko.ru/wp-content/uploads/2017/01/drugs-cause-disease.png" alt="Drugs that cause restless legs syndrome" width="608" height="369" srcset="" data-srcset="https://i1.wp..png?w=608&ssl=1 608w, https://i1.wp..png?resize=300%2C182&ssl=1 300w" sizes="(max-width: 608px) 100vw, 608px" data-recalc-dims="1">!} 
Treat the symptoms of tired legs disease promptly. Do not let the disease take its course, do not self-medicate, despite the apparent simplicity of the disease.
Bottom line - we learned from the article:
- what is restless legs syndrome causes and treatment
- who most often suffers from this disease
- found out the symptoms
- we know what to do with the syndrome to improve the quality of sleep
- What are the traditional and folk methods of treating the problem?
Healthy and calm feet to you! Have a great sleep!
Restless legs syndrome (RLS) is a sensorimotor disorder characterized by unpleasant sensations in the lower extremities that appear at rest (usually in the evening and at night), force the patient to make movements that relieve them and often lead to sleep disturbances. RLS was first described by Thomas Willis in 1672, but systematic study of the syndrome began only in the 40s of the 20th century with the work of the Swedish neurologist K. A. Ekbom, in whose honor RLS was named Ekbom syndrome.
Epidemiology
Current population studies indicate that the prevalence of RLS in adults is 5-10%, with symptoms occurring at least once a week in approximately two-thirds of cases and more than twice a week in one-third of cases, significantly affecting quality of life. RLS occurs in all age groups, but is more common in middle and old age (in this age group its prevalence reaches 10-15%). However, at least a third of RLS cases first appear in the second or third decades of life. RLS occurs 1.5 times more often in women than in men, and this disproportion is further exacerbated by the fact that women are more likely to seek medical help for RLS. According to a number of researchers, approximately 15% of cases of chronic insomnia are associated with RLS.
Etiology
In more than half of cases, RLS occurs in the absence of any other neurological or physical disease (primary or idiopathic RLS). Primary RLS usually appears in the first three decades of life (SBP with early onset) and may be hereditary. In various clinical series of RLS, the proportion of familial cases ranged from 30 to 92%. Analysis of family cases indicates a possible autosomal dominant type of transmission with almost complete penetrance, but variable expressivity of the pathological gene. Both polygenic and monogenic nature of the disease are assumed. In some families, an association of RLS with loci on chromosomes 12, 14 and 9 has been identified. It is possible that in a significant proportion of cases the disease is multifactorial in nature, arising as a result of a complex interaction of genetic and external factors.
The three main causes of secondary (symptomatic) RLS are pregnancy, end-stage uremia, and iron deficiency (with or without anemia). RLS is detected in 15-52% of patients with uremia, including almost a third of patients on dialysis, almost 20% of pregnant women (symptoms often appear only in the 2nd-3rd trimester and disappear within a month after delivery, but sometimes persist ). In addition, cases of RLS have been described in diabetes mellitus, amyloidosis, cryoglobulinemia, vitamin B12 deficiency, folic acid, thiamine, magnesium, as well as alcoholism, thyroid diseases, rheumatoid arthritis, Sjögren's syndrome, porphyria, occlusive arterial disease or chronic venous insufficiency of the lower extremities. In many of these conditions, RLS occurs in conjunction with symptoms of axonal polyneuropathy. RLS has also been described in patients with radiculopathies, as well as with lesions of the spinal cord, usually in the cervical or thoracic regions (for example, with trauma, spondylogenic cervical myelopathy, tumors, myelitis, multiple sclerosis). Symptomatic RLS most often begins after age 45 (late-onset RLS) and usually tends to progress more rapidly.
RLS is sometimes detected in patients with Parkinson's disease, essential tremor, Tourette's syndrome, Huntington's disease, amyotrophic lateral sclerosis, post-polio syndrome, but it remains unclear whether this combination is due to chance (due to the high prevalence of RLS), the presence of common pathogenetic mechanisms, or the use of medicines.
Pathogenesis
The effectiveness of dopaminergic drugs and the possibility of worsening symptoms under the influence of antipsychotics indicate that a key element in the pathogenesis of RLS is a defect in dopaminergic systems. However, the nature of this dysfunction remains unclear. IN last years Using positron emission tomography (PET), patients with RLS revealed a moderate decrease in the uptake of [ 18 F]-fluorodopa in the putamen, which indicates dysfunction of dopaminergic neurons in the substantia nigra, but, unlike Parkinson's disease, the number of these neurons does not decrease. According to some authors, the leading role in the pathogenesis of RLS is played by dysfunction not of the nigrostriatal system, but of the descending diencephalic-spinal dopaminergic pathways, the source of which is a group of neurons located in the caudal thalamus and periventricular gray matter of the midbrain. This system regulates the passage of sensory impulses through the spinal cord and, possibly, segmental mechanisms of motor control.
The clear daily rhythm of the clinical manifestations of RLS may reflect the interest of the structures of the hypothalamus, in particular the suprachiasmatic nucleus, which regulates the daily cycles of physiological processes in the body. The increase in RLS symptoms in the evening can also be explained based on the dopaminergic hypothesis: the worsening coincides with a daily decrease in dopamine levels in the brain, as well as with the period of lowest iron levels in the blood (this indicator decreases by almost half at night). The association of RLS with iron deficiency may be determined by the important role of iron in the functioning of the dopaminergic system.
The occurrence of RLS in the setting of peripheral nervous system lesions suggests the importance of peripheral nervous system dysfunction in the generation of symptoms. According to the clinical picture, including the daily rhythm of symptoms and responsiveness to drugs, RLS associated with damage to the peripheral nervous system is not much different from primary RLS, which indicates their pathogenetic relationship. It is possible that in some patients with RLS, polyneuropathy, iron deficiency, coffee abuse or other factors only reveal an existing hereditary predisposition, which partly blurs the line between the primary and secondary variants of RLS.
Clinical picture
Clinically, RLS is characterized by two main groups of symptoms: subjective pathological sensations and excessive motor activity, which are closely related. Sensory symptoms of RLS include sensations of itching, scraping, stabbing, bursting or pressing, as well as the illusion of “crawling” sensations. Some patients complain of a dull cerebral or intense cutting pain, but more often these sensations are not painful, although they can be extremely painful and unpleasant. Painful pathological sensations experienced by patients are usually referred to as dysesthesias, non-painful ones - paresthesias, but the boundary between them is arbitrary. Pathological sensations with RLS initially have limited localization and most often occur in the depths of the legs, less often (as a rule, with polyneuropathy) - in the feet. With subsequent progression, they often spread upward, involving the thighs and arms, and occasionally the torso and perineal area. Unpleasant sensations usually occur on both sides, but in more than 40% of cases they are asymmetrical, and sometimes even unilateral.
A characteristic feature of pathological sensations with RLS is depending on motor activity and poses. They usually occur and intensify at rest (sitting and especially lying down), but decrease with movement. To alleviate their condition, patients are forced to stretch and bend their limbs, shake, rub and massage them, toss and turn in bed, get up and walk around the room, or shift from foot to foot. Each patient develops his own “repertoire” of movements that help him reduce discomfort in the limbs. During movement, the unpleasant sensations decrease or disappear, but as soon as the patient lies down, and sometimes just stops, they intensify again.
Symptoms of RLS have a clear circadian rhythm, appearing or intensifying in the evening and night hours. On average, they reach their maximum severity in the period from 0 to 4 am, and their minimum in the period from 6 to 10 am. Initially, most patients experience symptoms about 15 to 30 minutes after they go to bed. But subsequently, the time of their appearance may become earlier and earlier, right up to daytime hours. In severe cases, the characteristic circadian rhythm disappears and symptoms become permanent. They can occur not only in a supine position, but also in a sitting position and can make visiting a movie or theater, flying on an airplane, or a long trip in a vehicle unbearable.
A direct consequence of unpleasant sensations in the limbs and the need to constantly move is sleep disturbance - insomnia. Patients cannot fall asleep for a long time and often wake up at night. The consequence of insomnia is fatigue and decreased attention during the daytime. The complaint of poor sleep is the leading one for most patients, and it is this that most often brings them to the doctor. Many patients have comorbid depression.
Sleep disturbances in RLS are aggravated by periodic limb movements (PLM), which occur during sleep in 80% of patients with RLS. They are rhythmic short-term jerks, most often observed in the legs, are stereotypical and involve dorsiflexion of the big toes, sometimes with fanning of the remaining toes or flexion of the entire foot. In more severe cases, bending of the legs at the knees and hip joints. MPCs last from 0.5 to 5 s and occur in series at intervals of 20-40 s over several minutes or hours. In mild cases, neither the patients themselves nor their close relatives suspect the presence of PDC; they can only be detected using polysomnography. In severe cases, movements continue throughout the night and may cause frequent awakenings. In general, the intensity of MDCs correlates well with the severity of RLS manifestations, so their registration using polysomnography can serve as a reliable objective method for assessing the effectiveness of RLS therapy.
General and neurological examination of patients with primary RLS usually does not reveal any abnormalities. But with symptomatic RLS, signs of a somatic or neurological disease, primarily polyneuropathy, can be detected.
Course of the disease
In primary RLS, symptoms usually persist throughout life, but their intensity can fluctuate significantly - it is temporarily intensified during periods of stress, due to the consumption of caffeine-containing products, after intense physical activity, and during pregnancy. In most cases, there is a tendency for symptoms to slowly worsen over time. But sometimes there are periods of stationary course or remission, which can last from several days to several years. Long-term remissions are observed in 15% of patients. In secondary RLS, the course depends on the underlying disease. Remissions in symptomatic forms are rare.
Diagnostics
RLS refers to frequent illnesses, but is rarely diagnosed - mainly due to the low awareness of practical (practicing) doctors, who are often inclined to explain the complaints of patients with neurosis, psychological stress, diseases of peripheral vessels, joints, and spinal osteochondrosis. However, in most cases, the diagnosis of RLS is simple and is based on the patient’s complaints. The diagnostic criteria for RLS proposed by the International RLS Study Group are presented in the table.
RLS must be differentiated from akathisia, “painful legs - moving toes” syndrome, hypnic twitching, night cramps, meralgia paresthetica, polyneuropathy, fibromyalgia. Having diagnosed RLS, the secondary nature of the syndrome should be excluded by conducting a thorough neurological and somatic examination of the patient. The scope of laboratory and instrumental examination is dictated by the need to exclude polyneuropathy (including using electroneuromyography), anemia, uremia, diabetes mellitus, chronic lung diseases, rheumatic diseases, deficiency of iron, magnesium and vitamins. It should be noted that iron deficiency in the body is more reliably indicated by the level of ferritin, rather than serum iron. If there is a deviation from the typical clinical picture of the syndrome or if standard therapy is ineffective, polysomnography is indicated.
General principles of treatment
For symptomatic RLS, treatment should primarily be aimed at correcting the primary disease or replenishing the identified deficiency (iron, folic acid, magnesium, etc.). Correction of iron deficiency with the administration of iron supplements is indicated when serum ferritin levels are below 45 mcg/ml. Typically, ferrous sulfate (325 mg) is prescribed in combination with vitamin C (250-500 mg) 3 times a day between meals. In primary RLS, the basis of treatment is symptomatic therapy, with the help of which it is possible to achieve complete regression of symptoms in a significant proportion of patients. Symptomatic therapy includes both non-drug measures and the use of drugs.
Non-drug therapy
First of all, it is important to find out what medications the patient is taking and, if possible, discontinue those that may increase the manifestations of RLS (neuroleptics, metoclopramide, antidepressants - both tricyclic and selective serotonin reuptake inhibitors, lithium preparations, terbutaline, antihistamines and antagonists H2 receptors, nifedipine and other calcium antagonists).
All patients are recommended to do moderate physical activity during the day, following a certain bedtime ritual, evening walks, evening shower, balanced diet with refusal to drink coffee, strong tea and other caffeine-containing products (for example, chocolate or Coca-Cola) during the day and evening, limiting alcohol, stopping smoking, normalizing the daily routine.
Even Ekbom (1945) noted that the symptoms of RLS are more pronounced in patients with cold feet, while with an increase in body temperature they are alleviated. In this regard, a warm foot bath or a light warming foot massage before bed can significantly improve the condition. In some cases, transcutaneous electrical stimulation, vibration massage, darsonvalization of the legs, reflexology or magnetic therapy are effective.
Drug therapy
It is customary to prescribe medications for RLS in cases where it significantly disrupts the patient’s vital functions, causing persistent sleep disturbance, and non-drug measures are not effective enough. In mild cases, you can limit yourself to taking sedatives of herbal origin or prescribing a placebo, which can give a good, but sometimes only temporary effect.
In more severe cases, you have to choose a drug from four main groups: benzodiazepines, dopaminergic drugs, anticonvulsants, opioids.
Benzodiazepines accelerate the onset of sleep and reduce the frequency of awakenings associated with PDC, but have relatively little effect on the specific sensory and motor manifestations of RLS, as well as PDC. The most commonly used benzodiazepines are clonazepam (0.5-2 mg at night) or alprazolam (0.25-0.5 mg). With long-term use of benzodiazepines, there is a danger of developing tolerance with a gradual decrease in effect and the formation of drug dependence. The negative aspects of the action of benzodiazepines also include the possibility of developing or increasing drowsiness during the day, decreased libido, increased sleep apnea, episodes of confusion at night, as well as worsening cognitive impairment in the elderly. In this regard, benzodiazepines are currently used sporadically in mild or moderate cases - during periods of deterioration, and in severe cases requiring constant treatment, they are prescribed only when dopaminergic drugs are ineffective.
Dopaminergic drugs (levodopa and dopamine receptor agonists) are the mainstays of treatment for RLS. They affect all the main manifestations of RLS, including the maximum concentration limit. Dopaminergic drugs are so effective in RLS that a positive reaction to them can serve as an additional criterion for diagnosing RLS, and its absence, as, for example, in Parkinson's disease, should be considered a basis for revising the diagnosis. The effect of dopaminergic drugs in RLS occurs in doses that are significantly lower than those used in Parkinson's disease. Dopaminergic agents appear to be equally effective for both primary and symptomatic RLS.
Levodopa has been used for RLS since 1985, when its effectiveness in this category of patients was first shown. Currently, levodopa is prescribed in combination with DOPA decarboxylase inhibitors benserazide (Madopar) or carbidopa (Nakom, Sinemet). Treatment begins with 50 mg of levodopa (approximately 1/4 tablet of Madopar “250”), which the patient should take 1-2 hours before bedtime. If the effectiveness is insufficient, after a week the dose is increased to 100 mg, the maximum dose is 200 mg. Taking levodopa provides an adequate effect in 85% of patients. In many patients it remains effective for many years, and in some patients its effective dose may remain stable or even decrease. Levodopa is generally well tolerated by patients with RLS, and side effects(nausea, muscle spasms, tension headaches, irritability, dizziness, dry mouth) are usually mild and do not require discontinuation of the drug. Given the rapid onset of effect and the lack of need for dose titration, levodopa may be considered the treatment of choice for intermittent worsening symptoms.
However, when long-term use in a significant proportion of patients, the effectiveness of levodopa decreases, while the duration of action of a single dose is reduced to 2-3 hours, which may be followed by a rebound increase in the symptoms of RLS and PDC in the second half of the night. In this case, it is recommended to increase the dose of the drug or add a second dose immediately before bedtime or upon awakening at night. However, with an increase in the dose of levodopa, the rebound increase in symptoms may not be eliminated, but only shift to early morning hours, while its intensity may increase. Experience shows that a more reasonable alternative in this situation is to switch to a sustained-release levodopa preparation (Madopar GSS). A slow-release drug that acts over 4-6 hours and provides good dream throughout the night and prevents morning rebound intensification of symptoms.
In approximately half of patients, during long-term treatment with levodopa, symptoms gradually begin to appear earlier (sometimes even during the day), becoming more intense and widespread (the so-called “augmentation”). The higher the dose of levodopa, the stronger the augmentation, so increasing the dose of levodopa in this situation only makes the situation worse, completing a vicious circle. When using Madopar GSS as a basic therapy for RLS, rebound enhancement and augmentation are observed less frequently than when taking standard levodopa drugs. In this regard, Madopar GSS is now often used as a means of initial treatment of RLS (1-2 capsules 1-2 hours before bedtime). Sometimes it is reasonable to recommend to the patient 1 hour before bedtime 100 mg of levodopa as part of a standard drug or a soluble fast-acting drug, which provides a relatively rapid onset of effect, and 100 mg of levodopa as part of a slow-release drug (for example, 1 capsule of Madopar GSS). When augmentation develops, it is recommended to either replace levodopa with a dopamine receptor agonist, or add it to it (by reducing the dose of levodopa).
Dopamine receptor agonists (DRAs) have been used for RLS shortly after levodopa was shown to be effective, in 1988. Experience shows that the effectiveness of ADR for RLS is approximately equivalent to that of levodopa. ADRs can be considered as a means of choice if long-term daily medication is required. For RLS, both ergoline drugs (bromocriptine, cabergoline) and non-ergoline drugs (pramipexole, piribedil) are used. Non-ergoline drugs have the advantage of being free from side effects such as vasospastic reactions, pleuropulmonary, retroperitoneal fibrosis, and fibrosis of the heart valves. To avoid nausea, ADRs are taken immediately after meals and the dose is adjusted by slow titration. Pramipexole is initially prescribed at a dose of 0.125 mg, then gradually increased until the effect is achieved (usually no more than 1 mg). The effective dose of piribedil is 50-150 mg. For bromocriptine treatment, the starting dose is 1.25 mg and the effective dose ranges from 2.5 to 7.5 mg. Cabergoline treatment begins with 0.5 mg, and its effective dose is 1-2 mg. The indicated dose is usually prescribed once 1-2 hours before bedtime, but in severe cases, additional administration of the drug may be necessary in the early evening hours. Side effects when taking ADR include nausea, fatigue, headache, dizziness, daytime sleepiness. Domperidone may be prescribed at the beginning of treatment to prevent nausea.
With long-term use of ADR, signs of augmentation are detected in approximately 25-30% of patients, but they are almost never as severe as with levodopa treatment. If one of the ADRs turns out to be ineffective, you can try replacing it with another drug from this group. It is important to note that dopaminergic drugs, while eliminating the symptoms of RLS, do not always lead to normalization of sleep, which requires the addition of a sedative drug (benzodiazepine or trazodone).
It should be noted that, probably due to the absence of denervation and the normal number of dopaminergic neurons, dopaminergic drugs are effective in RLS at doses significantly lower than those used in Parkinson's disease. Moreover, side effects such as dyskinesia, psychosis, impulsivity, and compulsive behavior (common in Parkinson's disease) are extremely rare in RLS.
In those few cases where the patient does not tolerate dopaminergic drugs well, and benzodiazepines are ineffective or cause intolerable side effects, they resort to anticonvulsants or opioids. Of the anticonvulsants, gabapentin is currently most often used - at a dose of 300 to 2700 mg/day. The entire daily dose is usually prescribed once in the evening. Opioid drugs (codeine, 15-60 mg; dihydrocodeine, 60-120 mg, tramadol, 50-400 mg at night, etc.) can significantly reduce the symptoms of RLS and PDC, but the risk of developing drug dependence makes their use justified only in the most severe cases where all other treatment methods are ineffective. The treatment algorithm for RLS is shown in the figure.
For RLS, it is possible to use some other drugs (clonidine, folic acid, magnesium, vitamins E, B, C), but their effectiveness has not been confirmed in controlled studies. In some patients, amantadine, baclofen, zolpidem are effective; beta blockers (for example, propranolol) can reduce symptoms, but sometimes cause them to worsen.
Treatment of RLS has to be carried out over a long period of time over many years, and therefore it is very important to follow a unified treatment strategy. Sometimes it is carried out only during the period of intensification of symptoms, but often patients are forced to take certain drugs for life to maintain drug remission. It is better to start treatment with monotherapy, choosing a drug taking into account its effectiveness in each individual patient and the presence of concomitant diseases. If monotherapy is insufficiently effective or in cases where, due to side effects, it is not possible to achieve a therapeutic dose of one of the drugs, it is possible to use a combination of drugs with different mechanisms of action in relatively small doses. In some cases, it is advisable to rotate several drugs that are effective for a given patient, which allows them to maintain their effectiveness for many years.
Treatment of RLS in pregnant women is particularly challenging. None of the drugs commonly used for RLS are considered safe during pregnancy. Therefore, when RLS develops during pregnancy, they are usually limited to non-drug measures (for example, a walk and a warm shower before bed) and the administration of folic acid (3 mg/day), as well as iron supplements (if there is a deficiency). Only in severe cases is it permissible to use small doses of clonazepam, and if they are ineffective, small doses of levodopa.
Trazodone and monoamine oxidase inhibitors (MAOIs) can be used to treat depression in patients with RLS. Data on the effect of selective serotonin reuptake inhibitors in patients with RLS and PDC are contradictory. However, in some patients they can nevertheless improve the condition, which is explained by the suppression of the activity of dopaminergic neurons. Tricyclic antidepressants, like antipsychotics, are contraindicated.
Conclusion
RLS is one of the most common neurological diseases. Modern methods Treatments make it possible to achieve almost complete elimination of symptoms and a significant improvement in the quality of life in the vast majority of patients. In this regard, timely diagnosis of the syndrome is of key importance - doctors must learn to recognize, behind the seemingly “banal” complaints of patients about insomnia or discomfort in the legs, this is a very unique and, most importantly, curable disease.
Literature
Averyanov Yu. N., Podchufarova E. V. Restless legs syndrome // Neurological Journal, 1997. No. 3. P. 12-16.
Levin O. S. Restless legs syndrome // Diagnosis and treatment of extrapyramidal disorders / ed. V. N. Shtoka. M., 2000. pp. 124-138.
Levin O. S. Restless legs syndrome // Extrapyramidal disorders. Guide to diagnosis and treatment / ed. V.N.Shtoka, I.A.Ivanova-Smolenskaya, O.S.Levin. M.: Medpress-inform, 2002. P. 425-434.
Allen R. P., Walters A. S., Monplaisir J. et al. Restless legs syndrome // Slep. Med., 2003. V.4. P. 101-119.
Allen R.P. Contraversies and challenges in defining etiology and pathophysiology of restless legs syndrome // Am. J. Med., 2007. V.120. S. 13-21.
Becker P. M., Jamieson A. O., Brown W. D.. Dopaminergic agents in restless legs syndrome and periodic limb movements of sleep: response and complications of extended treatment in 49 cases // Sleep, 1993. V.16. P. 713-716.
Ekbom K. A. Restless legs // Acta Med. Scand., 1945. V. 158. P. 5-123.
Earley C. J. Restless legs syndrome // N. Engl. J. Med., 2003. V. 348. P. 2103-2109.
Happe S., Klosch G., Saletu B.. et al. Treatment of idiopathic restless legs syndrome (RLS) with gabapentin // Neurology, 2001. V.57. P. 1717-1719.
Kaplan P.W. Levodopa in restless legs syndrome // Ann Pharmacotherapy, 1992. V. 26. P. 244-245.
Montplaisir J., Godbout R., Poirier G.. et al. Restless legs syndrome and periodic movements in sleep: physiopathology and treatment with l-dopa // Clin. Neuropharmacol., 1986. V. 9. P. 456-463.
Montplaisir J., Nicolas A., Denesle R. et al. Restless legs syndrome improved by pramipexole // Neurology, 1999. V.52. P. 938-943.
Ondo W., Jankovic J. Restless legs syndrome. Clinicoetiologic correlates // Neurology, 1996. V. 47. P. 1435-1441.
Paulus W., Trenkwalder C. Pathophysiology of dopaminergic therapy - related augmentation in rextless leg syndrome // Lancet Neurology, 2006. V. 5. P. 878-886.
Phillips B., Young T., Finn L. et al. Epidemiology of restless legs symptoms in adults//Arch. Int. Med., 2000. V.160. P. 2137-2141.
Saletu M., Anderer P., Saletu-Zyhlarz G.. et al. Restless legs syndrome (RLS) and periodic limb movement disorder (PLMD) acute placebo-controlled sleep laboratory studies with clonazepam // Eur. Neuropsychopharmacol., 2001. V. 11. P. 153-161.
Silber M. H., Ehrenberg B. L., Allen R. P.. et al. An algorithm for the management of restless legs syndrome // Mayo Clin Proc., 2004. V. 79. P. 916-922.
Steiner J.C.. Clonidine helps restless legs syndrome // Neurology, 1987. V. 37(Suppl. 1). P. 278.
Trenkwalder C., Henning W. A., Walters A. S.. et al. Circadian rhythm of periodic limb movements and sensory symptoms of restless legs syndrome // Mov. Disord., 1999. V.14. P. 102-110.
Turjanski N., Lees A. J., Brooks D. J.. Striatal dopaminergic function in restless legs syndrome: 18F-dopa and 11C-raclopride PET studies // Neurology, 1999. V.52. P. 932-937.
Ulfberg J., Nystrom B., Carter N. et al. Prevalence of restless legs syndrome among men aged 18 to 64 years: anassociation with somatic disease and neuropsychiatric symptoms // Mov. Disord., 2001. V. 16. P. 1159-1163.
Walker S. L., Fine A., Kryger M. H.. L-DOPA/carbidopa for nocturnal movement disorders in uremia // Sleep, 1996. V.19.
P. 214-218.
O. S. Levin, Doctor of Medical Sciences, Professor
RMAPO, Moscow
One of the most distressing sensorimotor disorders known to neurology is restless legs syndrome. The disease is one of the main factors provoking chronic insomnia. The disorder affects all age groups, but is more common in older people. Women over 60 years of age are most prone to its occurrence. Differential diagnosis, despite the prevalence of the syndrome, is significantly difficult, and the correct diagnosis is established only in 8% of all patients.
Classification of the syndrome by type of manifestation
Traditionally, the disorder affects middle-aged and elderly people, but restless legs syndrome is also observed in children in some cases.
The disorder often accompanies pregnancy, causing the woman to develop severe and psychological disorders that are incompatible with healthy pregnancy.
- Childhood restless legs syndrome. The disorder in children is often mistakenly classified as so-called “growing pains.” Some clinical studies have found that restless legs syndrome in childhood is associated with lack of attention from parents, and as a result, psychological disorders.
Other doctors believe that the disorder occurs in response to children's motor hyperactivity during the day. The true unambiguous causes of childhood and adolescent deviation have not yet been established, however, it has been proven that this syndrome tends to progress over the years and does not disappear on its own.
- Syndrome in pregnant women. The disorder occurs during pregnancy in 15-30% of cases. Often its onset occurs in the third trimester, and then the syndrome disappears on its own during the first month of motherhood. However, it is necessary to understand that the disorder can be directly related to problems in the body, including iron deficiency anemia.
- Idiopathic restless legs syndrome. This form refers to the primary manifestation of the disorder. In this case, the syndrome manifests itself in the first 30 years of life and has a hereditary etiology of the autosomal dominant type.
Clinical signs are no different from the symptomatic (secondary) syndrome, however, the idiopathic form is characterized by the absence of concomitant somatic and neurological diseases.
If the syndrome is caused by pathological factors, it can be transmitted genetically from mother to child. To dispel doubts about the physiological causes of the disease, you need to seek help from doctors.
Do you know the feeling of numbness and “running” goosebumps in your legs? If these are isolated cases that are associated, for example, with an uncomfortable position of the legs, there is no need to worry. When this happens constantly, and the attacks are repeated, then, most likely, we can talk about the first
The concept of synkinesis is widespread not only in neurology, but is also quite often used in speech therapy. On the website you can find out more about this pathology.
Causes and provoking factors of the disorder
The symptomatic syndrome is observed mainly in the middle and older age categories, arising for the following reasons:
- Iron-deficiency anemia;
- Insulin-dependent diabetes mellitus type 2;
- Chronic hypovitaminosis of folic acid and cyanocobalamin;
- Uremia;
- Kidney and heart failure;
- Discogenic radiculopathy;
- Complications resulting from gastrectomy;
- Hormonal imbalance;
- Thyroid dysfunction: hypothyroidism, hyperthyroidism or thyrotoxicosis;
- Sjögren's syndrome;
- Obstructive diseases of the lung tissue;
- Venous insufficiency of the legs;
- Rheumatoid arthritis;
- Diseases of the blood vessels;
- Porphyrin disease;
- Cryoglobulinemia;
- Severe spinal cord injuries.
Pregnancy also contributes to the development of the disorder, but if no other pathological factor has provoked the syndrome, it is eliminated after the woman gives birth.
Polyneuropathic causes:
- Porphyritic polyneuropathy;
- Amyloidosis.
Symptoms of the syndrome
 Symptoms of the disorder are distinguished by a clearly limited time frame.
Symptoms of the disorder are distinguished by a clearly limited time frame.
The disorder manifests itself in a certain daily rhythm, and the peak of symptoms occurs between 00.00 and 04.00 at night.
A person suffering from restless legs syndrome experiences a combination of the following symptoms:
- Intense pain in the lower extremities;
- The pain is often associated with a feeling of strong tingling, burning, a feeling of fullness and tightness, itching, pain in the legs;
- Unpleasant sensations are localized in the area of the ankle joint and calf muscles;
- Occurs mainly at night;
- Signs begin to progress in a state of complete rest;
- Discomfort and pain tend to decrease with physical activity;
- Rhythmic movements in the legs of a neuropathic nature.
The clinical consequence of the development of restless legs syndrome in the vast majority of cases is severe insomnia. The patient cannot sleep for a long time due to increased motor activity and pain in the lower extremities.
If this is still possible, the patient wakes up after a short time from increasing symptoms, and falling back into sleep becomes almost impossible for him.
Differential diagnosis
Like any neurological disease, restless legs syndrome undergoes careful medical analysis before an accurate diagnosis is made.
Diagnostics consists of several main stages:
- A thorough study of the patient’s symptoms and an objective assessment of his family history;
- Somatic and neurological face-to-face examination;
- Blood chemistry;
- Study of ferritin content in blood serum based on tests;
- Electroneuromyography;
For additional data on the presence of concomitant diseases, you may need to consult a therapist and endocrinologist.
General computerization has led to the widespread spread of a disease that manifests itself as pain and discomfort in the hands. To eliminate it, various techniques are used, including surgery.
Tumors are characterized by various manifestations, which depend on their size and location. About the main symptoms of neuroblastoma in children, you will find
Doctors call cerebral edema a fairly common complication after a stroke. You can find out why it develops by following the link.
Treatment for restless legs syndrome
Therapeutic measures
After an adequate diagnosis has been made and the underlying cause of the disease has been identified, comprehensive treatment is prescribed.
First of all, it may be associated with correcting a deficiency in the blood of certain substances and taking multivitamin complexes containing folic acid, magnesium and iron. In any case, the attending physician decides how to treat this syndrome.

Drug treatment
Includes various drugs:
- Tranquilizers and sleeping pills (Restoril, Ambien, Halcion, Klonopin). Used when mild form diseases;
- Antiparkinsonian drugs. To date, Mirapex treatment has proven itself to be excellent. The drug stimulates the synthesis and metabolism of dopamine, activates its receptors in the striatum.
It is completely absorbed 1-2 hours after administration and has a rapid effect. Indicated for the symptomatic treatment of idiopathic restless legs syndrome and Parkinson's disease. It must be prescribed by a doctor, as it has a number of contraindications and side effects;
- Anticonvulsants (Neurontin, Tegretol);
- Opiates. Injections of potent opiate-containing injections are used in particularly severe cases of the syndrome. The following drugs are used: Codeine, Methadone, Oxycodone, Propoxyphene;
- Creams and ointments for pain relief and general relaxation (Nise, Relax, Menovazin, Nicoflex).
Physiotherapy
The following are used as incentive measures:
- Endodermal electrical stimulation;
- Darsonvalization of limbs;
- Magnetotherapy;
- Vibromassage;
- Acupuncture;
- Therapeutic applications with sea mud;
- Lymphopress;
- Manual acupressure;
- Cryotherapy.
Psychotherapy
Consultations and work with a psychotherapist. May be necessary if no other common causes of the disorder have been identified.
Some patients require correction of comorbid mental disorders by taking antidepressants, sedatives and benzodiazepine receptor agonists (Zolpidem, Trazodone).
Homeopathic remedies
- Zincum Metallicum;
- Zincum C6;
- Zincum Valerianicum;
- Sodium Bromatum.
Folk remedies

- Massage using bay oil. You can prepare the product by infusing 30 g bay leaf in 100 g vegetable oil. Treat your feet daily before bed;
- Rubbing with concentrated tincture of golden mustache;
- Phytotherapeutic foot baths with the addition of nettle, sage, valerian and oregano;
- Rub your shins with apple cider vinegar;
- Taking tea with linden and lemon balm;
- Drinking hawthorn infusion;
- Cold and hot shower.
Physiotherapy
Includes a number of exercises:
- Mandatory load on the legs during the day. Ideally, classic squats without a load;
- Stretching gymnastics - basic exercises to stretch the calf muscles;
- Long jogging or long-distance walking before bed;
- Exercising with an exercise bike or cycling;
- Leg flexion and extension;
- Walking on toes with high knees.
Treatment at home
- Increased intellectual stress;
- Self-massage of the calf muscles and legs;
- Alternating cold and hot foot baths;
- Correction of nutrition and giving up bad habits;
- Compliance with sleep hygiene rules.
Everything about causes of inflammation of the sciatic nerve, as well as about the methods of its treatment and preventive measures.
It happens that the acoustic neuroma does not respond to conservative treatment, then surgery is resorted to. How the patient’s postoperative period progresses, you will find in
Restless legs syndrome causes and treatment (RLS) is today's hot topic for study and is of interest to those who are bothered by it.
What is this restless leg syndrome, and why does it keep us from sleeping peacefully until the morning? Is it possible to get rid of this syndrome forever?
Restless legs syndrome causes and treatment, what kind of disease it is:


Medicine has determined that this syndrome is a neurological disorder. The older you get, the higher the risks. Women are more susceptible to this disease than men.
A person simply needs to move his legs, he has such an alarming need. This sensation is not very painful, but occurs deep inside the legs. They are described as a kind of tension inside the muscles. Sometimes the arms and the entire torso are involved in this process.
As soon as the patient moves, all symptoms disappear. The movement of the legs stops, and everything starts again. Unfortunately, these symptoms only worsen at night, weaken a little during the day, but do not disappear completely.
Restless legs syndrome, symptoms:
Patients describe their sensations in their legs or arms, especially at rest before bed:
- They start to get sick.
- It's as if someone is crawling on them.
- They start to burn.
- It pierces like an electric current.
- They begin to itch and tingle.
- Feeling of tingling, bursting, squeezing.
- Worms crawling under the skin.
- Coldness in the legs or, conversely, the feeling of boiling water pouring into the legs.
There is a desire to move your legs, and not only at night, but also during the day, when a person is simply resting. Occurs every ten to fifteen seconds at rest.
Sometimes leg symptoms are very difficult to describe. It is good if the doctor knows enough about this disease. No changes were found on MRI or other examinations. Blood is normal.
Almost a person cannot sleep peacefully. Even if the patient has fallen asleep, the legs continue to twitch, which means the brain’s reaction does not stop. The person does not rest normally.
During the day he is lethargic, tired, and sometimes the patient walks around with suicidal thoughts. Treatment in this condition is urgent.
It is not at all uncommon for symptoms to suddenly disappear without a trace. Apparently the cause of the trigger for restless legs syndrome disappears.
It often torments women during pregnancy, especially in the second or third trimester.
The following are believed to be guilty:
- Deficiency of vitamins and of course minerals (folic acid, iron).
- Insomnia.
- Modified hormonal background pregnant woman.
- Increased sensitivity of the body.
Simple exercises, walks, a calm environment, and proper nutrition can help.
- A complex of vitamins and minerals is prescribed.
- Warm baths at night.


Primary or idiopathic:
The beginning of its development is usually considered before the age of 40 or from childhood. The reason is genetics. Continues for the rest of your life. Not associated with any disease.
Secondary or symptomatic:
The cause of restless legs syndrome is another, underlying disease in a person. Starts after 45 years, suddenly.
Symptoms of the disease progress.
Restless legs syndrome causes:
The following diseases are considered to be the causes of restless legs syndrome in humans:
- Diabetes mellitus (peripheral polyneuropathy).
- Acute lack of iron in the body.
- Failure of the kidneys and heart.
- Joint disease: rheumatoid arthritis.
- Pregnancy.
- Neuropathy.
- Abuse of drinks containing caffeine.
- Taking certain medications.
- Long and intense physical activity.
- Spinal cord damage.
- Disturbance of the thyroid gland in a patient.
- State of chronic stress.
- Chronic lung diseases.
- Use of nicotine and alcohol.
Antidepressants (serotonin reuptake inhibitors) can also provoke restless legs syndrome.
To confirm the diagnosis:
- Neurography.
- Polysomography.
- Artography (using sensors on the lower leg and foot).
- Encephalogram.
- Rectromyography.
Restless legs syndrome treatment:


- Healthy lifestyle: nutrition with big amount vitamins, fiber, greens.
- Play sports (any), but in moderation.
- At night, massage or warm baths for relaxation.
- Contrasting foot baths are good.
- A pillow between your legs helps.
- Classes (asanas for relaxation).
- When doing physical education, do more exercises for the leg muscles.
- Eliminate extreme fatigue for a better night's rest.
- Fight in a well-ventilated bedroom.
- Try to go to bed in the evening and get up in the morning at the same time.
- Less light before main sleep.
- Eat foods rich in magnesium (nuts, leafy vegetables, whole grains).
- After lunch, do not drink coffee, tea, or sugar.
- Give up the habit of smoking and drinking alcohol.
- Drink enough clean water.
Medicines:
Dopaminergic drugs:
- Bromocriptine.
- Levodopa: about an hour before bedtime, two capsules of Madopar.
- Pramipexole: one hour before bedtime 0.25 mg to 1 mg.
- Pergolide.
- Rotigotine.
- Carbidopa.
- Mirapex: at a dose of 0.25 mg in the evening.
Well relieves symptoms of anxious leg movements during sleep. But they have side effects: insomnia, swelling of the limbs, bloating, nausea, chest pain.
Usually these medications are not prescribed for a long time. During treatment, you cannot abruptly stop taking medications, only gradually reduce the dose. Drug withdrawal syndrome is observed.
Iron and folic acid, magnesium supplements:
- At night, two Magnerot tablets.
- Ibuprofen for mild symptoms.
Anticonvulsants:
- Neurontin.
- Gabapentin: from 300 to 2700 mg at night.
Benzodiazepines:
- Restoril.
- Clonazepam.
- Temazepam.
- Klonopin.
Opiates in severe cases:
- Codeine.
- Propoxyphene.
For neurological causes and symptoms of restless legs syndrome, antidepressants and tranquilizers are prescribed.


It’s better to buy 50 grams of the following herbs at the pharmacy:
- Valerian root.
- Horsetail grass.
- Meadowsweet leaves and flowers.
- Hawthorn: fruits.
- Rose hips: fruits.
- Motherwort grass.
- Melissa herb.
- Peppermint.
Take two tablespoons (without top) of the mixed mixture. Brew with 600 grams of boiling water. Wrap up and leave for up to one hour. We drink 300 grams before lunch and before bed.
At exactly 7 pm, take a Mirapex 0.25 mg tablet.
Too many patients simply forget about the symptoms of restless legs. They sleep peacefully and their quality of life improves.
In conclusion, I would like to add that restless legs syndrome causes and treatment depend on the person’s attitude to the underlying disease of the body.
If you have diabetes, you need to actively treat it, following all the doctor’s instructions, starting with diet and ending with physical exercise.
Only then can you avoid negative consequences, and therefore restless legs syndrome. Everyone needs to sleep at night and get enough sleep.
Get treatment and get well.
I always look forward to seeing you on my site. Come back often.
Watch a video about restless legs syndrome: