Temperature from antipsychotics. When taking pills is harmful, or neuroleptic malignant syndrome. Symptoms and signs
Movement disorders accompany many diseases - both somatic and affecting the human psyche. They differ in a variety of clinical manifestations and forms. One of the most common is neuroleptic syndrome, which accompanies the incorrect use of certain drugs. Antipsychotic drugs are capable of causing a variety of movement disorders, which, for ease of diagnosis and therapy, are combined into single group.
In the acute course of such a violation, treatment consists in the abolition of the medication that caused the appearance of the condition. However, if the tool is used long time, then the formation of life-threatening complications is possible, which is not always possible to cope with.
Reasons for the development of neuroleptic syndrome
The problem is identified as a complication of taking drugs that affect the work of the central nervous system. In rare cases, drugs that do not affect the cerebral cortex can also cause symptoms. The neuroleptic syndrome is caused by the following factors:
- A history of neurological disease increases the risk of developing the disease. This is due to the already present violations of the work of neurons and the aggravation of the situation when taking medications.
- The main reason for the occurrence of such symptoms is the use of neuroleptics. These drugs are common in psychiatry for the relief of the main manifestations of disorders of the higher nervous activity. They should be used carefully, according to the instructions and instructions of the doctor.
- A substance such as metoclopramide, which is part of the drug "Cerukal", is used in the fight against vomiting. With incorrect dosing, it can provoke the development of a malignant form of neuroleptic syndrome, the treatment of which is not always possible.
Classification and main features
The first symptoms of the lesion are diagnosed both within 2-3 hours after taking the appropriate drugs, and several days after the start of the course. The clinical picture reaches its maximum manifestation within 14–30 days. The classic signs of neuroleptic syndrome are the triad of muscle rigidity-fever-mental abnormalities. However, the symptoms of this disorder are varied. There are special medical recommendations for the diagnosis and interpretation of such pathologies. The literature also describes a certain sequence of trait development. Initially, muscle stiffness occurs, after which an elevated body temperature forms within a few hours. This is presumably due to changes in metabolic processes. The last recorded mental abnormalities, expressed in drowsiness or arousal. In severe cases, patients suffer from delusions and hallucinations.
Changes in the work of neurons also affect the functions of the cardiovascular system. A person's blood pressure rises, rapid heart rate, tachypnea and increased sweating occur. In the absence of treatment, the maximum intensity of manifestations is recorded on the third day.
Bradykinesia
Similar symptoms are formed against the background of taking antipsychotics, and clinical signs are recorded during the first week of using drugs. Most common in the elderly. Speech disorders, anxiety and aggressiveness are noted, less often - depression and depression, as well as difficulty in movements. It is difficult for the patient to control the work of the muscles, and therefore he needs help to move.
parkinsonism
This type of syndrome is the most common. A few years ago, such consequences of taking antipsychotics were considered normal and, according to many doctors, testified to the success of the therapy. Today it is known that this assumption is erroneous. Voluntary movement disorder, which is the main symptom of Parkinson's disease, occurs with the use of certain antipsychotics. In patients, muscle tremor is recorded, fine motor skills worsen, movements become slow and constrained. With the timely cancellation or dose reduction of drugs, the neuroleptic syndrome disappears and does not cause complications, since the body manages to remove the compound from the blood without loss of neuronal function. However, in the case of chronic disorders, such a clinical picture persists in a person until the end of life and leads to disability.
Acute dystonia
This process is characterized by an abrupt onset. It is formed against the background of taking antipsychotic drugs, and a complication may occur already on the first day of using the drug. At the same time, in most cases, the formation of an acute condition is facilitated by existing violations of work. internal organs accompanied by endocrinopathies, metabolic imbalance and neurological problems. More often, dystonia is diagnosed in young males. It is manifested by spasms of the muscles of the neck, and the movement disorder also affects facial expressions. Patients involuntarily make grimaces, throw back their heads. Gradually, the process spreads to the entire body. A person takes strange and uncomfortable postures, wriggles. In this case, the arms and legs remain uninvolved. Spasms of skeletal muscles are so strong that they are accompanied by intense pain and provoke the formation of sprains and dislocations. Relief of attacks is achieved by symptomatic treatment and the abolition of antipsychotics.
Akathisia
This disorder, unlike the previous one, is more typical for women. This clinical picture is formed both at the initial stage of the use of the corresponding drugs, and during their long-term use. These neuroleptic problems are especially common with an incorrect dosage of medications in the direction of increasing the amount of the active substance. In rare cases, they represent a neuroleptic withdrawal syndrome. Patients complain of a persistent and increasing feeling of discomfort or pain. They suffer from a strong need to actively move and seek a comfortable position. It is difficult for such a person to sit still. Symptoms may disappear spontaneously. Often, such a disorder is combined with neuroleptic depression, since it causes severe discomfort to the patient.
Malignant neuroleptic syndrome
A prolonged course of the disorder leads to an aggravation of the clinical picture. In many cases, it becomes impossible to negate the consequences of pathology. Patients develop such a dangerous condition as malignant neuroleptic syndrome. The complication is most typical when taking drugs that block dopamine receptors. The whole difficulty in the fight against this disease lies in the irreversibility of the ongoing changes. Even with the provision of timely and urgent care, the recovery of the patient remains in question. The symptoms of this type of neuroleptic syndrome are similar to the manifestations of such problems as ischemic cerebral stroke, malignant tumor lesions, severe poisoning and sepsis. This complication ends in death in 15% of cases.
Diagnostics
Accurate methods to confirm the neuroleptic syndrome do not exist today. Since in most cases the clinical picture is provoked by taking medications, their cancellation has a positive effect on the patient's well-being. Unfortunately, this method is not always applicable, because in the case of a malignant course of the process, fast medical care is required. Doctors resort to symptomatic therapy and stabilization of the person's condition, after which a thorough history is taken to determine the list of drugs taken by the victim.
Hematological tests, as a rule, are nonspecific and only indicate damage to muscle tissue, as well as the development of an inflammatory reaction. Instrumental and visual diagnostic methods also do not give significant results.
Treatment
The main fight against neuroleptic syndrome is the abolition of the drug that caused the development of pathology. After the drug is removed from the body, movement disorders also disappear. To alleviate the patient's condition, symptomatic therapy based on the use of tranquilizers is used. These drugs reduce muscle tone and promote relaxation, and also have a sedative effect. The most popular are Diazepam, Lorazepam and Chlordiazepoxide.
Treatment shows good results when the patient is hospitalized. In specialized institutions, staff are able to provide proper care, as well as mobile assistance. In stationary conditions, electrolyte disturbances are also corrected by intravenous infusions. This contributes to a more rapid excretion of metabolic products of neuroleptics and improves the patient's condition. To control daily diuresis, a urethral catheter is required. With a serious increase in temperature, antipyretics and non-steroidal anti-inflammatory drugs are used. Antioxidants are also used, such as Mexidol, which protect the nervous tissue from the negative effects of insufficient oxygen concentration in the blood. If during an attack of convulsions the patient hurt himself, then after stabilization of the condition, an operation for osteosynthesis or reposition of fractures and dislocations may be required.
Forecast and prevention
The outcome of the disease depends on the timeliness of medical care and the individual characteristics of the patient. With the rapid abolition of neuroleptics, it is possible to avoid complications of the condition. Prevention comes down to following the recommendations of the doctor and monitoring the condition of the person taking antipsychotics.
Malignant neuroleptic syndrome (syn. MNS) is a pathological condition that develops against the background of long-term use psychotropic substances (neuroleptics or antipsychotics). It is noteworthy that the disease can develop even in completely healthy person who, for any reason, has been prescribed these medications.
In addition to the irrational use of medicines, among the predisposing factors are severe exhaustion, addiction to alcohol, dehydration, the course of infectious processes and other diseases.
The disease has a large number of external signs, but the main ones are muscle rigidity, fever, mental disorders and fluctuations in blood tone.
Diagnosis requires the passage of a wide range of laboratory tests, and instrumental procedures and activities carried out by the clinician are of a secondary nature.
Treatment consists in the abolition of all drugs and the use of conservative therapeutic methods. Quite often they resort to such a procedure as artificial ventilation of the lungs.
Etiology
Malignant neuroleptic syndrome differs in that it is considered an extremely rare disease. The main reason for the development of pathology lies in the inadequate use of drugs - non-compliance with the recommendations of the attending physician or their intake for no apparent reason.
List of drugs with this side effect:
- typical and atypical antipsychotics from various groups;
- "Cerukal";
- "Metoclopramide";
- "Reserpine";
- "Tetrabenazine";
- lithium preparations;
- antidepressants;
- "Dozipin";
- "Fenelzin";
- "Desipramine".
Other negative external factors, including antipsychotic treatment options:
- high dosage of antipsychotics;
- rapid rise daily allowance drugs;
- the use of a highly potent substance;
- use of a long-acting drug;
- intramuscular administration of drugs;
- abrupt withdrawal of the drug;
- simultaneous use of several substances;
- electroconvulsive therapy;
- high temperature and humidity environment.
Predisposing sources can be:
- severe dehydration;
- chronic alcoholism;
- lack of iron;
- physical exhaustion;
- mental retardation;
- encephalopathy of post-traumatic nature;
- with Lewy bodies;
- pathologies leading to brain failure;
- previous traumatic brain injury and infectious lesions of the central nervous system;
- psychomotor agitation;
- the course of allergic processes;
- violations of water and electrolyte balance;
- problems with the functioning of the thyroid gland;
- the presence of catatonia and birth trauma in history;
- affective psychosis.
Most often, the diagnosis is established in persons of two age categories: from 20 to 50 years old and starting from 70 years old. It should be noted that males are more likely to suffer from the disease.
Malignant neuroleptic syndrome has an insufficiently clear pathogenesis. Clinicians consider several hypotheses:
- problems with dopamine metabolism in the central nervous system;
- peripheral effect of neuroleptics.
Classification
Pathology has several options for the course:
- acute form - characterized by the sudden onset of symptoms, a sharp deterioration in a person's condition and high probability the development of coma, the duration of the phase is approximately 14 days;
- chronic form - develops in cases where the treatment of the previous form was completely absent.
The disease has several degrees of severity:
- mild - expressed in a slight increase in temperature, tachycardia, fluctuations in blood pressure and an affective-delusional state;
- moderate - the main symptoms are aggravated, the development of stupor, speech and motor disorders is possible;
- severe - there is a critical change in laboratory parameters, complete immobilization and flaccid stupor, there is a high probability of coma and other complications that can lead to death.
Symptoms
The disease has specific and rather pronounced clinical manifestations that simply cannot be ignored. First symptoms:
- tremor of the limbs;
- convulsive seizures;
- increase in temperature indicators;
- instability of blood tone values;
- delirium;
- frequent mood swings.
As the neuroleptic malignant syndrome progresses, it will be expressed by the following signs:
- muscle hypotension - muscle weakness, which develops in 97% of patients, the severity may vary from mild increased tone to the symptom of "lead pipe" (resistance to any movements is noted);
- urinary incontinence;
- painful pallor of the skin;
- psychomotor agitation;
- increased heart rate;
- profuse salivation;
- shuffling gait;
- white coating in the language;
- dry mucous membranes;
- sunken eyes;
- reduced skin turgor;
- confusion of thought;
- violation of the process of swallowing food;
- syndrome restless legs;
- increased sweating;
- the appearance of specific rashes - blisters have different sizes, are filled with serous-hemorrhagic fluid and can be localized on the buttocks, heels, knees and elbows;
- increased anxiety and irritability.
In some cases, a coma or catatonic stupor develops.
Diagnostics
The main diagnostic criteria are laboratory data, but the process of clarifying the correct diagnosis should have an integrated approach.
The neurologist must independently carry out several manipulations:
- to study the medical history - to look for a disease, the treatment of which could include the use of antipsychotics or any of the above drugs;
- to collect and analyze a life history - to state the fact of the use of medicines for no apparent reason;
- conduct special neurological tests;
- measure temperature, heart rate and blood pressure;
- assess the condition of the skin;
- to interview the patient in detail (if the person is conscious) or his relatives - to determine the first time of onset and the severity of symptoms, which will indicate the severity of the disease.
Among the laboratory studies it is worth highlighting:
- general clinical blood test;
- blood biochemistry;
- immunological and hormonal tests;
- determination of the gas composition of the blood;
- microscopy of the fluid that fills the skin rashes, and cerebrospinal fluid;
- toxicological screening of urine;
- liver tests;
- study of the serum of a biological fluid.
Instrumental diagnostics is limited to the following procedures:
- CT and MRI of the head;
- ultrasonography;
- lumbar puncture;
- chest x-ray.
Before starting treatment, it is necessary to conduct a differential diagnosis. Malignant neuroleptic syndrome should be distinguished from such pathologies:
- heatstroke;
- severe infections;
- malignant;
- neoplasm of the brain;
- prolonged crush syndrome;
- lethal catatonia;
- serotonin syndrome;
- tumor of the central nervous system;
- severe course of dystonia;
- acute intoxication with drugs, alcohol or chemicals;
- withdrawal states;
- autoimmune disorders.
Treatment
Therapy should be aimed at the immediate cessation of taking drugs that provoked the onset of characteristic symptoms.
Treatment consists of conservative methods:
- taking medications;
- provision of adequate nutrition;
- courses therapeutic massage;
- implementation of physiotherapy procedures.
May be required:
- installation of a urinary catheter;
- intubation;
- artificial ventilation of the lungs;
- use of a nasogastric tube;
- hemodialysis;
- plasmapheresis;
- electroconvulsive procedures.

Drug therapy involves the use of such drugs:
- dopamine agonists;
- nootropic substances;
- iron preparations;
- benzodiazepines;
- neuroleptic correctors;
- medicines to relieve symptoms, such as antipyretics, pain relievers, and other drugs.
The goals of the above therapeutic measures:
- normalization of the patient's well-being;
- elimination of muscle rigidity;
- prevention of complications;
- hydration.
Possible Complications
Malignant neuroleptic syndrome is a life-threatening disease because it leads to the following complications:
- rhabdomyolysis;
- epilepsy;
- neuronal cerebral degeneration;
- acute renal or hepatic failure;
- sudden cardiac death;
- mental disorders;
- generalized allergic reaction.
Prevention and prognosis
Specific preventive measures are aimed at competently using any medications, i.e., only as prescribed by the attending physician and with the obligatory observance of the daily rate and duration of therapy.
Do not forget about the regular passage of a complete preventive examination in a medical institution - this will identify diseases that increase the likelihood of the formation of neuroleptic syndrome.
As for the prognosis, the outcome is often unfavorable. This is due to late seeking qualified help and the formation of complications, which often lead to death. When such a diagnosis is confirmed, every third patient dies. Even with timely therapy, the mortality rate is 10%.
Is everything correct in the article from a medical point of view?
Answer only if you have proven medical knowledge
Inflammation of the lungs (officially pneumonia) is an inflammatory process in one or both respiratory organs, which is usually infectious in nature and is caused by various viruses, bacteria and fungi. In ancient times, this disease was considered one of the most dangerous, and although modern treatments allow you to quickly and without consequences get rid of the infection, the disease has not lost its relevance. According to official figures, in our country every year about a million people suffer from pneumonia in one form or another.
The disease, which is characterized by the formation of pulmonary insufficiency, presented in the form of a massive release of transudate from the capillaries into the lung cavity and, as a result, contributing to the infiltration of the alveoli, is called pulmonary edema. talking in simple terms, Pulmonary edema is a condition when fluid stagnates in the lungs, seeping through the blood vessels. The disease is characterized as an independent symptom and can be formed on the basis of other serious ailments of the body.
Almost all neuroleptics, including atypical ones, can cause NMS, but most often it is caused by antipsychotics belonging to the groups of butyrophenones, phenothiazines and thioxanthenes, in particular haloperidol, fluphenazine (moditen) and chlorpromazine (chlorpromazine).
Other external factors, including those related to antipsychotic treatment options Factors related to the physiological state of patients
In addition, some researchers include the state of confusion and delirium, the diagnosis of affective psychosis, male gender, and advanced age as risk factors. Other researchers note that this complication most often affects young and middle-aged people - from 20 to 40 (or up to 50) years. Some authors talk about an asymmetric bipolar distribution of cases of NMS according to the age of patients: the first peak occurs in the period of 20-40 years, the second - in persons over 70 years of age.
Malignant neuroleptic syndrome can develop at any time after the start of treatment or an increase in the dose of an antipsychotic (from several hours to days, months and years), but the onset of the syndrome during the first 24-72 hours is more typical. In 2/3 cases, NMS develops in the first week of treatment, in most cases - in the first 14 or, according to other authors, 30 days from the start of therapy.
Prevalence
Data on the incidence of NMS among patients treated with antipsychotics are conflicting. Most authors define it within 0.02-3.23%, T. Benzer (2010) - at 12.2%.
There are indications that the use of high-potency antipsychotics causes MNS in 0.5-3.2% of patients, and low-potency drugs cause this complication much less often - more than 2 times, in 0.02-1.4% of cases.
Pathogenesis
According to the first, most common hypothesis, blockade of central dopaminergic receptors (mainly D2 receptors) in the striatum and hypothalamus by neuroleptics causes muscle rigidity, which is the basis for the increase in temperature and hypermetabolism. Decrease in dopamine also regulates serotonergic structures in the striatum and hypothalamus responsible for thermoregulatory processes. In addition, it is assumed that antipsychotics cause blockade diencephalospinal system and that this leads to disinhibition of segmental neurons of the sympathetic nervous system and the development of tachycardia, tachypnea, arterial hypertension.
According to another hypothesis, the cause of muscle rigidity and the subsequent increase in temperature is peripheral dopamine blockade, causing increased contraction. skeletal muscle due to genetic predisposition, due to a complex of changes, such as increased calcium metabolism in muscle tissue due to its increased intake through activated calcium channels and / or release from the sarcoplasmic reticulum; mitochondrial oxidation disorder; activation of calmodulin; shifts in the metabolism of glucose and cholesterol. This process is also similar to the pathophysiological mechanisms of the development of malignant hyperthermia and reveals the genesis of rhabdomyolysis in neuroleptic malignant syndrome. A direct toxic effect of neuroleptics on skeletal muscle tissue, which causes its rigidity, has also been established.
In addition to these hypotheses, a number of researchers attach great importance sympathoadrenal hyperactivity and autonomic dysfunction in the pathogenesis of neuroleptic malignant syndrome.
Clinical picture
It is characterized by disorders in the neurological, mental and somatic spheres. The main clinical manifestations of NMS: muscle rigidity, fever (hyperthermia), vegetative changes, mental disorders.
Usually, the symptoms of neuroleptic malignant syndrome last an average of 7-14 days, but can stretch for up to 30 days. When using prolong drugs, the duration of this condition doubles.
Muscle rigidity and other neurological manifestations
progressive muscle rigidity- one of the most significant signs of NMS. She, as well as other extrapyramidal disorders, are observed in neuroleptic malignant syndrome in 97% of patients. This is the first and early symptom a disease that in most patients precedes a rise in temperature, although sometimes the severity of both symptoms increases simultaneously.
The severity of muscle rigidity is different - from muscle hypertonicity to the "lead pipe" symptom, when there is extreme resistance to passive movements. If neuroleptic malignant syndrome is due to the use of atypical antipsychotics, extrapyramidal symptoms, including muscle rigidity, are less pronounced, may be absent at the onset of an attack or not develop at all.
In addition, the following extrapyramidal disorders can be observed with NMS: brady- and akinesia, cog wheel symptom, myoclonus, tremor, chorea, opisthotonus, dysarthria, aphonia, dysphagia, akathisia, dystonia (trismus, blepharospasm, oculogeric crisis), epileptiform seizures, hyperreflexia, stop clonus, nystagmus and opsoclonus, discoordination. Because of the shuffling, mincing gait, in some cases there is difficulty in walking. Neurological effects sometimes remain for months or years after recovery from neuroleptic malignant syndrome.
A direct consequence of muscle rigidity is an increase in body temperature.
Hyperthermia
The second of the main signs of NMS is observed in 95-98% of patients (according to other sources - 34%).
The temperature is most often febrile: 38.5-42 ° C. Rare cases of atypical neuroleptic malignant syndrome with little or no fever have been described.
Vegetative shifts
Somatic disorders in neuroleptic malignant syndrome caused by dysfunction of the autonomic nervous system are diverse: tachycardia and other cardiac dysrhythmias, arterial pressure lability, tachypnea, skin pallor, sweating, salivation, urinary incontinence. There are symptoms of dehydration: dry mucous membranes, sunken eyes, decreased skin turgor, furred tongue.
Mental disorders
One of the early and very frequent manifestations of neuroleptic malignant syndrome; occur immediately after the development of muscle rigidity and / or fever and are observed in 97% of patients.
Mental shifts in NMS are varied: from anxiety, confusion, agitation or delirium to oneiroid and amental clouding of consciousness, severe catatonia, akinetic mutism, stupor and coma. Fluctuations in the level of impaired consciousness are often observed. The stupefaction with mutism that develops in NMS often resembles lethal catatonia.
It is often difficult to make a differential diagnosis between the mental manifestations of the underlying disease, for which antipsychotic therapy was performed, and disorders caused by the development of MNS.
Laboratory data
Laboratory data are of great importance for the correct diagnosis of this syndrome. Patients with NMS have:
Complications and causes of death
The following complications of neuroleptic malignant syndrome are most dangerous:
- acute respiratory failure: pulmonary embolism, aspiration pneumonia, pulmonary edema , adult respiratory distress syndrome (shock lung)
- cardiac pathology: arrhythmias, acute myocardial infarction, sudden cardiac arrest
- epileptiform seizures
- infectious complications: colibacillary fasciitis, sepsis, urinary infections
- deterioration of mental state after the abolition of antipsychotics
- cerebral neuronal degeneration
Rhabdomyolysis is a direct consequence of severe muscle rigidity, and its occurrence is also facilitated by dehydration due to the immobility of patients due to mental disorders and related eating difficulties. It gives rise to acute renal failure, which is observed in NMS in 50% of patients and very often leads to death.
Cause acute respiratory failure is often pulmonary embolism accounting for about 25% of all deaths from neuroleptic malignant syndrome. The basis of the pulmonary embolism that occurs with this syndrome is hyperthermia and the dehydration of the body associated with it, as well as the immobility of patients due to catatonic stupor or their prolonged fixation during arousal.
Another common cause respiratory failure is aspiration pneumonia, the occurrence of which is associated with mental disorders, inhibition of the cough reflex, dysphagia, increased salivation.
Pulmonary edema in rare cases, it can also complicate the course of neuroleptic malignant syndrome and lead to death. The development of pulmonary edema is associated with an increase in pressure in the pulmonary capillaries due to hypertension in the pulmonary circulation due to sympathetic hyperactivity.
Cause respiratory distress syndrome serves as rigidity of the muscles of the chest and / or rhabdomyolysis, while hypoventilation, dyspnea, severe hypoxia occur.
To the deadly cardiac pathology include various arrhythmias. Cases of acute myocardial infarction and sudden cardiac arrest are described, as well as reversible cardiomyopathy, simulating the clinical picture of myocardial infarction.
A rare complication of NMS is epileptiform seizures due to high fever. DIC is associated with a disorder rheological properties of blood due to severe shifts in homeostasis in neuroleptic malignant syndrome.
Significant causes of death include infectious complications: colibacillary fasciitis due to deep bedsores, urinary infections due to catheterization Bladder, sepsis.
Morphological changes in the brain that occur along the course of NMS are represented by neuronal degeneration, which is more often due to hyperpyrexia, hypoxia, etc. than neuroleptic malignant syndrome as such. As a result of these disorders, surviving patients may remain cognitive impairment, dementia, parkinsonism, dyskinesia, ataxia.
Causes of death in NMS also include refractory acidosis And multiple organ failure. Russian authors pay great attention to the description of skin toxic-allergic reactions that complicate the course of NMS, but these complications are usually not mentioned in English-language sources.
Diagnostics
Malignant neuroleptic syndrome can be represented by a single symptom, a complex of symptoms, or an extended clinical picture. The severity of symptoms varies significantly between patients.
There are no generally accepted clear diagnostic criteria for neuroleptic malignant syndrome. DSM-IV-TR gives the following diagnostic criteria:
A. Muscle rigidity and fever developed during antipsychotic therapy.
B. Sweating, dysphagia, tremor, urination disorder, altered consciousness, mutism, tachycardia, increased or lability blood pressure, leukocytosis, increased serum CPK.
Symptoms of groups A and B must not be caused by other causes (C): neurological diseases taking other medications. And also - psychoses with catatonic symptoms (D). For a diagnosis of NMS, both of group A and at least two of group B must be present in the presence of conditions C and D.
The diagnosis of NMS is a "diagnosis of exclusion": it is made after the exclusion of another pathology that may lead to a similar clinical picture. To confirm this disease, in addition to a thorough clinical examination and a careful study of the anamnesis (including family history), it is necessary to conduct the following laboratory tests:
Differential Diagnosis
to diseases and pathological conditions with which it is necessary to differentiate neuroleptic malignant syndrome include:
Serotonin syndrome, malignant hyperthermia and lethal catatonia cause the greatest difficulties in the differential diagnosis of NMS.
Particularly difficult is the differential diagnosis of NMS and lethal catatonia, sometimes they are even considered one disease. However, lethal catatonia develops independently of the use of antipsychotics and begins with the onset of mood swings, affective disorders, and severe psychotic arousal, while the onset of NMS is associated with antipsychotic therapy and is characterized by severe extrapyramidal symptoms, including muscle rigidity.
J. Schröder et al. suggest to differentiate these conditions to evaluate the response to the abolition of antipsychotics: in case of NMS it causes positive changes, in case of lethal catatonia the effect is minimal, negative dynamics is more often observed. J. Strawn et al. consider that symptoms such as parkinsonian phenomena, high fever and stupor, which developed after taking medication, most likely indicate in favor of NMS, rather than lethal catatonia.
The most significant differences between NMS and serotonin syndrome: serotonin syndrome is characterized by a sudden early start(within 24 hours after the start of taking or changing the dosage of the drug); symptoms - agitation, diarrhea, dilated pupils, myoclonus, hyperreflexia; rare mortality (23 recorded deaths from 2003 to 2003); neuroleptic malignant syndrome is characterized by a slower onset (most often within 7 days after starting or changing the dose); symptoms - dysphagia, salivation, urinary incontinence, hyperthermia (> 38 ° C), akinesia, muscle rigidity up to the "lead pipe" symptom, rhabdomyolysis; frequent mortality (in 15-20% of cases according to 2003 data).
Treatment
The most important condition for the successful treatment of neuroleptic malignant syndrome is its early diagnosis. Treatment should be carried out in a specialized hospital (ward intensive care, intensive care unit) and should be complete, up to the normalization of all indicators and the complete disappearance of symptoms. Prehospital care is also important, including symptomatic therapy: the use of anti-anxiety drugs (for example, benzodiazepines; physical restraints should be avoided in NMS), attention to the state of the respiratory tract, respiratory and circulatory functions.
In a specialized hospital, the first and most important step in treatment is the abolition of all antipsychotics or other medications that have caused the development of the syndrome. If NMS develops as a response to a dose reduction or withdrawal of drugs in the treatment of Parkinson's disease, the use of these drugs should be immediately resumed and thereafter should be reduced gradually. Subsequent medical measures include: a) symptomatic therapy; b) medicinal treatment; c) electroconvulsive therapy (ECT). These measures are applied separately or in combination, depending on the nature and severity of the syndrome.
Supportive (symptomatic) therapy
Includes:
- hydration
- temperature drop
- aspiration prevention
- prevention of deep thrombosis
- good nutrition
In many cases, the abolition of antipsychotics and adequate symptomatic therapy leads to a reduction in the symptoms of NMS.
In case of violation of breathing and swallowing, intubation and artificial ventilation of the lungs are necessary, the introduction nasogastric tube for feeding and drug administration.
In the state of dehydration observed in most patients, it is necessary to carry out active rehydration of the body: massive intravenous administration of appropriate solutions. Parenteral infusions are also useful in order to eliminate hypotension - in particular, intravenous drip of sodium nitroprusside. In addition, nitroprusside, being peripheral vascular dilator, improves the patient's condition, enhances heat transfer and reduces fever. Useful and therapy with short-term antihypertensive agents: for example, nifedinin or oxygen.
If possible, monitoring of the work of the heart should be ensured.
When signs of rhabdomyolysis appear, it is necessary, due to the risk of developing renal failure, to increase hydration and achieve alkalinization of urine by intravenous administration of sodium bicarbonate solution. The placement of an indwelling urinary catheter helps monitor diuresis.
With developed renal failure, hemodialysis is indicated, which, however, is ineffective for the elimination of neuroleptics, since they are closely associated with blood proteins.
Fever control measures are very important, since hyperthermia leads to hypermetabolism and multiple organ failure. Physical methods contribute to lowering the temperature (cold wraps, icing over areas of large vessels, evaporation cooling) and the use of antipyretics. There is a point of view that heat generation in NMS is associated exclusively with muscle rigidity and cannot be corrected by conventional pharmacological means, therefore, in order to combat fever, medications to relieve muscle rigidity should be used.
To increase peripheral vasodilation, which enhances heat transfer, massage is indicated.
The prevention of aspiration should play an extremely important role: muscle rigidity in NMS can be the cause of the loss of gag and cough reflexes. It is necessary to check the presence of reflexes more often, carry out parenteral nutrition, ensure the position of the patient in bed, which prevents aspiration. Chest physiotherapy, some movement exercises, frequent turning or changing the patient's posture should be used to alleviate immobility and muscle rigidity. Due to the risk of aspiration in thoracic or esophageal dystonia, drugs should not be taken orally but should be administered parenterally or through a nasogastric tube.
For the prevention of deep thrombosis and pulmonary embolism, subcutaneous administration of heparin or small doses of lovenox is used. (English) Russian , for the same purpose, special elastic antithrombotic stockings can be used.
Careful attention should be paid to the nutrition of patients: most patients cannot eat on their own due to mental disorders or muscle rigidity with spasm of the esophagus; in addition, with NMS, patients lose a lot of energy due to fever and prolonged muscle rigidity. good food helps to minimize rhabdomyolysis and other tissue damage.
In cases of total muscle rigidity with life-threatening hyperthermia, anesthesia and general muscle relaxation can save the patient.
Drug treatment
Before initiating NMS pharmacotherapy, it is important to correctly assess its risks and benefits, and this should not be rushed; on the other hand, specific drug treatment for neuroleptic malignant syndrome is usually effective during the first few days of illness, and a long-term outcome is unlikely to be seen. Usually, the decision to prescribe a specific pharmacotherapy is made within 3 days. If NMS symptoms worsen, medical treatment should not be delayed.
Pharmacotherapeutic recommendations for NMS are based only on uncontrolled pro- and retrospective studies, as well as on individual case reports - therefore, information about the effectiveness of medical treatment of this disorder may be illusory. However, an extensive literature review by P. Sakkas et al. shows that drugs such as bromocriptine, amantadine, and dantrolene are most effective in treating the syndrome. Other researchers note that the use of these drugs almost halved the mortality from NMS and shortens the duration of the disease.
In patients with iron deficiency, it is advisable to prescribe iron preparations as an integral part of the standard therapy for NMS, since iron deficiency in the body contributes to the development of severe motor disorders, including this syndrome.
Electroconvulsive therapy (ECT)
It is used in severe, resistant to drug treatment cases. Particularly indicated for high temperature, impaired consciousness and profuse sweating, as well as with severe catatonic symptoms. Improvement usually occurs after several sessions (6 to 10).
Prevention of NMS after an episode
If the psychiatric disorders for which neuroleptic therapy was performed require its resumption after an episode of NMS, re-treatment with antipsychotics should be carried out only with the complete disappearance of all symptoms of the complication. The researchers recommend a period of 6 weeks to 5 days before resuming antipsychotics after complete resolution of symptoms (this depends, in particular, on whether antipsychotics were previously administered orally or parenterally). It is recommended to obtain the consent of patients and their relatives before re-treatment with antipsychotics, and all the advantages and disadvantages of such a decision should be discussed with patients and their relatives in detail.
The resumption of therapy should take place under the strictest clinical supervision to prevent recurrence of neuroleptic malignant syndrome.
Repeated use of antipsychotics in the same parameters as before the development of the complication leads to its relapse in 30-80% of cases. Therefore, a small dose of a low-potency neuroleptic of a different chemical class than the one that caused ECT should be chosen for the sample. Increasing the dose of an antipsychotic to a therapeutically effective level should be gradual and slow. The use of atypical antipsychotics is recommended, although the possibility of developing this complication from them is emphasized. Benzodiazepines are advised to relieve arousal during the resumption of therapy.
Under these conditions, the risk of recurrence of the complication is reduced to 10-13%.
During antipsychotic therapy, it is important to monitor the level of creatine phosphokinase in order to recognize a possible relapse as early as possible.
Malignant neuroleptic syndrome (epidemiology, risk factors, clinic, diagnosis, pathogenesis, therapy)
Epidemiology
Malignant neuroleptic syndrome (NMS), first described by J. Delay et al. (1960), is one of the most dangerous complications of neuroleptic therapy. Mortality in NMS, according to various authors, depending on the use of certain methods of treatment, ranges from 2.94 to 38% of cases. Prior to 1980, mortality in NMS was estimated at an average of 28-30%. After 1980, there has been a decrease in mortality in NMS to an average of 10-11.6%.
The frequency of development of NMS, according to foreign publications, ranges from 0.02% to 3.23% of all patients hospitalized in a hospital who were prescribed antipsychotic therapy. IN last years most authors point to a decrease in the incidence of NMS. For example, Gelenberg A. et al. (1988, 1989) note that NMS developed in 1 out of 1470 patients treated with antipsychotic therapy, which is 0.07% of all patients treated with antipsychotics. Keck P. et al. (1991) describe 4 (0.15%) cases of NMS that occurred during the period of treatment with neuroleptics in 2695 patients.
A retrospective epidemiological study conducted by the authors on the material of one of the largest psychiatric hospitals in Moscow - the Clinical Psychiatric Hospital No. P.B. Gannushkin, showed that during the year the development of NMS is observed in 2-4 patients. During the period from January 1, 1986 to December 31, 1995, NMS developed in 19 (0.02%) of 78,708 patients receiving antipsychotic therapy. At the same time, a lethal outcome occurred in 2 (10.5%) of 19 patients.
Risk factors for NMS
Risk factors for NMS remain poorly understood. It is known that NMS can develop in the treatment of neuroleptics in patients of different age groups and both sexes. Most often, NMS develops in middle-aged people. According to D.I. Malina (1989), who observed 77 cases of NMS - 32 (41.6%) people were men and 45 (58.4%) were women. Persons of young and middle age prevailed, 60% were over the age of 30 years. Most often, NMS developed when prescribing antipsychotics with a pronounced general and selective antipsychotic effect and high extrapyramidal activity - haloperidol, triftazin, thioproperazine. At the same time, the possibility of developing NMS was also noted in the treatment with neuroleptics that do not cause pronounced extrapyramidal effects. side effects, such as thioridazine, clozapine, as well as in the treatment of the atypical antipsychotic risperidone. With the use of depot antipsychotics, NMS is much more severe and lasts longer.
A number of authors believe that the rapid increase in the dose of antipsychotics and the parenteral route of their administration increases the risk of developing NMS, although others do not note the relationship between the incidence of NMS and the method of drug administration. It is assumed that the risk of developing NMS increases with the appointment of long-acting antipsychotics (for example, fluphenazine - decanoate).
Numerous cases of the development of NMS are described, when patients, along with antipsychotics, took antiparkinsonian drugs, and cases when correctors were not prescribed. Thus, the use of antiparkinsonian correctors does not prevent the development of NMS.
There was no definite pattern in the timing of the development of NMS from the start of antipsychotic therapy. NMS usually develops within the first 3-4 weeks from the start of antipsychotic treatment. In more than one third of cases, the development of NMS could be associated with a rapid increase in the dose of antipsychotics or the addition of new drugs with more powerful antipsychotic effects and high extrapyramidal activity, for example, when haloperidol is added to chlorpromazine. The possibility of developing NNS after a sudden cessation of taking psychotropic drugs was noted.
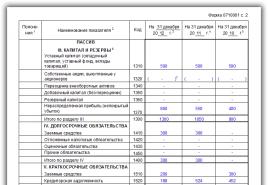
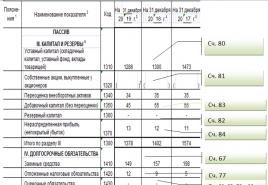
Rice. 1. Change in body temperature in patients with NMS during application various methods therapy, p(T1-T3)<0,05
Rice. 2. Change in muscle tone, assessed by the Simpson-Angus scale with the use of various methods of therapy in patients with NMS, p(T1-T3)<0,05, p(T1-T3)<0,001, p(T2-T3)<0,001

Table. Comparative effectiveness of various methods of NMS therapy
| Type of therapy | Number of patients | Mortality | Severity of the course (points) М±m | Duration of NMS | Severe complications accompanying NMS | |
| Abs. | % | |||||
| Infusion (control group) | 19 | 2 | 10,5 | 2.1±0.1 | 15.05±1.7 | Pneumonia - 4 (21.05%) patients |
| Infusion + bromocriptine | 10 | 1 | 10 | 1.8±0.09 | 11.9±2.15 | Pneumonia - 2 (20%) patients |
| Infusion + dantrolene | 10 | 0 | 0 | 1.8±0.1 | 6.9±1.16* | |
| p(1,3)<0,05 | No | |||||
| p(2,3)<0,1 | ||||||
| * The severity of the course of NMS was established on the basis of a total assessment of the severity of somatic disorders, psychopathological disorders and laboratory changes (on a three-point scale). | ||||||
According to most researchers, NMS can develop in patients with various forms of mental pathology, with neurological diseases and in mentally healthy individuals when prescribing antipsychotics and drugs that selectively block D2-dopamine receptors in the brain. However, NMS most often develops during neuroleptic therapy in patients with schizophrenia, affective disorders, and schizoaffective psychosis. According to B.D. Tsygankov (1997), all patients with NMS had paroxysmal current forms of schizophrenia - recurrent and paroxysmal-progredient (according to ICD-9 criteria). The results of our observations showed that all patients with NMS were diagnosed with schizophrenia or schizoaffective disorder before the development of complications.
According to J. Delay and P. Deniker (1968), who first described NMS, the development of complications was more often observed in individuals with a history of cerebro-organic hazards (traumatic brain injury, mental underdevelopment due to perinatal pathology). According to J. Levenson (1985), based on an analysis of 50 cases of NMS described in the world literature over a five-year period, signs of cerebral organic failure in history occurred in 17 (34%) patients. A special controlled study conducted by D.I. Malin (1989) to identify risk factors for the development of MNS, showed that in patients with MNS in the anamnesis, unconditionally brain hazards (birth trauma, asphyxia, traumatic brain injury, infectious diseases of the central nervous system, etc.) and conditionally brain hazards are significantly more common ( toxicosis of pregnancy in the mother, prematurity, heart defects, hypertension, rheumatism, etc.). In patients with NMS, antenatal and perinatal hazards also predominated in anamnesis, which indicated the presence of an early organic CNS lesion. In addition, patients with NMS had a history of signs of neurocirculatory dystonia and allergic reactions more often, which, in the author's opinion, indicates weakness of the diencephalic structures of the brain and a special "hyperergic" background.
A number of authors believe that physical exhaustion and dehydration can cause intolerance to antipsychotics and contribute to the development of NMS. It is also assumed that the high ambient temperature and humid climate increase the risk of complications.
Clinic and diagnosis of NMS
The clinical picture of NMS is characterized by the development of generalized muscle rigidity with central hyperthermia, clouding of consciousness with the development of stupor, and impaired homeostasis with severe dehydration. Characteristic changes in the blood formula are found (acceleration of ESR, lymphopenia, moderate leukocytosis without a stab shift), as well as an increase in the activity of transaminases and creatine phosphokinase in the blood plasma.
There are also tremors, extrapyramidal symptoms, dyskinesias, dysphagia, salivation, hyperhidrosis, tachycardia, increased and unstable blood pressure (BP), pallor of the skin. According to D.I. Malina (1989), the earliest sign of NMS, important for the early diagnosis of complications, is the appearance of extrapyramidal symptoms with a simultaneous exacerbation of psychosis according to the extrapyramidal-catatonic type with a predominance of pronounced catatonic disorders in the clinical picture (stupor with catalepsy and negativism).
The course and outcome of NMS largely depend on how quickly the complication was diagnosed, neuroleptics were canceled and maintenance therapy was prescribed, as well as on the associated somatic complications of infectious and inflammatory origin (pneumonia, cystitis, pyelonephritis). A prognostically unfavorable factor is the addition of bullous dermatitis, characterized by the appearance of blisters of various sizes in places subject to compression - the lumbosacral region, heels, elbows. Bubbles filled with serous-hemorrhagic contents quickly burst, and in their place bedsores form with areas of necrosis, which quickly suppurate and can lead to the development of sepsis. The possibility of such a complication, according to our data, is 10-15%. The appearance of bullous dermatitis is accompanied by a sharp deterioration in the condition of patients with an increase in hyperthermia and a disorder of homeostasis. Some authors consider bullous dermatitis as an independent severe complication of neuroleptic therapy not within the framework of the NMS.
The results of our own studies showed that, depending on the severity of clinical manifestations and the severity of laboratory changes, various variants of the course of NMS can be distinguished.
For a mild variant of the course of NMS, the following signs are characteristic: a rise in temperature to subfebrile numbers, moderate somatovegetative disorders (tachycardia up to 100 beats per 1 min, fluctuations in blood pressure within 150/90-110/70 mm Hg) and shifts in laboratory parameters ( increase in ESR to 18-30 mm/h, normal or slightly reduced number of lymphocytes from 15 to 19%). There are no violations of homeostasis and hemodynamic changes. The psychopathological picture is determined by affective-delusional or oneiroid-catatonic disorders.
The course of moderate NMS is characterized by an increase in body temperature to febrile numbers (38-39? C), pronounced somatovegetative disorders (shortness of breath with tachycardia up to 120 beats per 1 min), significant changes in laboratory parameters (increased ESR up to 35-50 mm / h , leukocytosis up to 10Ј109 / l, a decrease in the number of lymphocytes up to 10-15%). Moderately pronounced hypovolemia and hypokalemia, an increase in the level of transaminases and creatine phosphokinase in the blood plasma are noted. The psychopathological picture is determined by disorders of consciousness of the oneiroid and amental-like levels. Catatonic symptoms are represented by stupor with negativism or numbness, with the appearance in the evening of episodes of excitation with impulsivity, speech and motor stereotypes.
In severe cases of NMS against the background of hyperthermia, which can reach hyperpyrectic figures, there is an increase in somatovegetative disorders (tachycardia reaches 120-140 beats per 1 min, shortness of breath up to 30 breaths per 1 min), water-electrolyte disturbances increase, hemodynamic disorders increase, maximum shifts are found in laboratory parameters (increased ESR up to 40-70 mm / h, leukocytosis up to 12Ј109 / l, a decrease in the number of lymphocytes up to 3-10%, a significant increase in the level of alanine and aspartic transaminases, creatine phosphokinase in blood plasma). Clouding of consciousness can reach amental, soporous and comatose levels. Stupor with numbness and negativism is replaced by non-purposeful, limited to the limits of the bed, chaotic excitement or sluggish stupor with a decrease in muscle tone, and in extremely severe cases - complete immobility with areflexia.
It should be noted that the selection of variants of the course of NMS according to the degree of severity was conditional, since the severity of the course is a dynamic concept. In fact, the selected variants of the course of NMS were stages in the development of complications. Depending on the prognostically unfavorable factors, the adequacy of the therapy, the addition of somatic diseases, the course of NMS can stop at any of the identified stages.
Diagnosis of NMS is based on the appearance of the main symptoms of the complication associated with the use of antipsychotics, as described earlier, as well as characteristic changes in the blood (accelerated ESR, lymphopenia, moderate leukocytosis without stab shift). The DSM-IV provides the following criteria for the diagnosis of NMS.
A.
The development of severe muscle rigidity, including catatonic, with a simultaneous increase in body temperature against the background of antipsychotic therapy.
IN. The presence of two or more of the following concomitant symptoms: sweating, impaired swallowing, tremor, impaired urination, change in consciousness from delusional to coma, mutism, tachycardia, increased or unstable blood pressure, leukocytosis, increased activity of creatine phosphokinase.
WITH. Symptoms of group A and B should not be due to the development of any neurological disease (viral encephalitis, vascular or volumetric CNS damage), as well as the use of other drugs that can give symptoms similar to NMS (phencyclidine, amphetamines, monoamine oxidase inhibitors, blockers of dopaminergic structures). and etc.)
D. Symptoms of group A and B should not be the result of psychopathological conditions occurring with catatonic symptoms (catatonic form of schizophrenia, affective disorders with catatonic symptoms).
To exclude infectious-inflammatory and neurological diseases, all patients should undergo a thorough dynamic somatic, neurological and laboratory examination. In order to objectify the diagnosis, in addition to the general and biochemical blood tests, urinalysis, especially in controversial cases, it is necessary to conduct studies of the cerebrospinal fluid, to carry out blood cultures for sterility. Fluoroscopy and chest X-ray should be done to rule out inflammatory respiratory disease that could be the cause of the fever. The infectious-inflammatory genesis of the febrile reaction can be indicated by specific inflammatory changes in the blood count - high leukocytosis with a stab shift, as well as rapid normalization of body temperature after the appointment of antibiotic therapy.
In contrast to NMS, neurological infectious diseases (viral encephalitis, meningitis), vascular and volumetric lesions of the central nervous system are characterized by a pronounced complication of focal neurological symptoms, as well as the predominance of cerebral symptoms (drowsiness, stunning, stupor, coma, delirious disorders of consciousness). To exclude a volumetric CNS lesion in controversial cases, it is necessary to conduct electroencephalographic and M-ECHO studies, as well as computed tomography.
Pathogenesis of NMS
The pathogenesis of NMS remains unexplored to date. Most researchers explain the development of complications by the blockade of dopaminergic structures in the basal ganglia and hypothalamus, and not by the direct toxic effect of antipsychotics. A number of researchers explain the development of hyperthermia - the main symptom of NMS - by peripheral mechanisms, namely the appearance of muscle rigidity and the development due to this hypermetabolic status in muscle tissue, leading to increased heat production.
It is assumed that immunological disorders and an increase in the permeability of the blood-brain barrier, leading to neurosensitization of the body with subsequent autoimmune damage to the CNS and visceral organs, play an important role in the pathogenesis of NMS. Homeostasis disturbances occurring at a certain stage of the course of NMS, primarily water and electrolyte balance, are one of the main reasons for the development of severe hemodynamic disorders, deep disorders of consciousness, leading to death.
Our recent studies have shown that sympathoadrenal and serotonin hyperactivity plays an important role in the pathogenesis of NMS with an increase in the content of norepinephrine and serotonin in the blood plasma and a decrease in the concentration of the precursor of dopamine -3,4-dioxyphenylalanine.
Treatment of NMS
Treatment of NMS begins with the immediate withdrawal of antipsychotics and the appointment of intensive infusion-transfusion therapy aimed at correcting the main parameters of homeostasis: water and electrolyte balance, hemodynamics, acid-base state, protein composition, coagulation and rheological properties of blood. Treatment is carried out according to the principles of intensive care with round-the-clock drip infusions into the central or peripheral vein. One of the main tasks of infusion therapy is to combat dehydration and restore electrolyte balance. J. Delay, P. Deniker (1968), having first described the clinical manifestation of NMS, proposed therapeutic measures aimed at its correction. They pointed out that restoring fluid and electrolyte balance with the introduction of a large amount of fluid can prevent death. According to our data, the volume of intravenously administered fluid, depending on the degree of dehydration, can vary from 2.5 to 6 liters per day. Infusion therapy begins with replenishing the volume of circulating blood and improving its rheological properties with the help of protein and plasma-substituting solutions - dry and fresh frozen plasma, albumin, as well as solutions of polyglucin and rheopolyglucin. Along with these drugs, hemodez is administered, which has the strongest detoxifying effect. Further correction of the water and electrolyte balance is carried out by infusions of saline solutions, 5% glucose solution, potassium chloride. Most often, a 5% or 10% glucose-insulin-potassium mixture is used, which has the highest ability to utilize glucose and potassium. Nootropics, vitamins of groups B and C are also prescribed, Relanium, sodium oxybutyrate, hexenal are used to stop arousal.
In addition, attempts are being made to optimize the treatment of NMS in accordance with the existing hypotheses of its pathogenesis. So, first of all, the appointment of a D2-dopamine receptor agonist is recommended.
bromocriptine.
The drug is usually administered orally through nasogastric tubes at a dose of 7.5 to 60 mg per day.
Another drug recommended for the treatment of NMS is a muscle relaxant calcium channel blocker of the sarcoplasmic reticulum of striated muscle tissue - dantrolene. The recommended dose of the drug is 1 to 2 mg per 1 kg of the patient's body weight. It was noted that the appointment of dantrolene in the complex therapy of NNS is effective in most patients.
Our comparative study on the effectiveness of the use of bromocriptine and dantrolene in the complex therapy of NNS showed that dantrolene is the most effective drug. Its use in combination with intensive infusion therapy contributes to a significant increase in the effectiveness of treatment, a decrease in the duration and severity of NMS, and the prevention of deaths. Bromocriptine was prescribed at a dose of 15 mg per day, dantrolene - 100 mg per day. The results of the comparative study conducted by the authors are presented in the table and fig. 12.
There are a significant number of publications that discuss the possibility and effectiveness of ECT in the treatment of NMS. The effectiveness of ECT in NMS is associated with the effect on the diencephalic region, followed by the mobilization of the catecholamines norepinephrine and dopamine in the CNS. Under the condition of early diagnosis and timely withdrawal of antipsychotics, some authors point to the possibility of a critical reduction in the manifestations of NMS in the next 1-2 days from the start of ECT. Analysis of the world literature, conducted by S.Mann et al. (1990), showed that the positive effect of ECT occurred in 20 (74%) of 27 patients with NMS. J.Davis et al. (1991) reported that out of 29 cases of NMS treated with ECT, a positive effect occurred in 24 (83%) cases. The authors also reported that ECT reduced mortality in NMS from 21% to 10.3%.
According to D.I. Malina (1989) and B.D. Tsygankova (1997), the additional use of ECT against the background of intensive infusion therapy can significantly increase the effectiveness of the treatment of NMS. The use of ECT as a whole leads to faster relief of the complication, reduces the duration of its course by more than 2 times. At the same time, the effectiveness of therapy primarily depends on the initial severity of the patient's condition and, mainly, on the depth of the altered consciousness. In cases where illusory-fantastic and oneiroid-catatonic disorders dominate in the status of patients, the effectiveness of ECT is quite high. If the status of patients is dominated by amental disorders against the background of pronounced changes in homeostasis, ECT is ineffective and may lead to a deterioration in the condition of patients.
The use of plasmapheresis in the complex therapy of NMS is effective. According to D.I. Malina (1997), the effectiveness of plasmapheresis in NMS is associated with the ability of this treatment method to quickly stop the manifestations of endotoxicosis with the restoration of homeostasis of general and immunobiological reactivity and the elimination of toxic active metabolites of a biochemical and immune nature from the body of patients (lipid peroxidation products, "medium" molecules , auto- and antidrug antibodies, circulating immune complexes). Mortality in patients with NMS who, in addition to intensive infusion therapy, were prescribed plasmapheresis, was, according to the author, 2.4% (1 out of 24 patients) compared with 10.7% in the group of patients with NMS who were prescribed only intensive infusion therapy.
Conclusion
In the article, we tried to summarize the data of world literature and the results of our own scientific research on the problem of NMS.
NMS is a rare but extremely dangerous complication of antipsychotic therapy, leading in some cases to death in patients with endogenous psychoses. The significance of its clinical manifestations and the basic principles of therapy are important, first of all, for practitioners who may encounter the development of NMS in the course of neuroleptic therapy in mentally ill patients.
Literature:
1. Caroff S. The neuroleptic malignant syndrome. 1980; 41(3): 79-83.
2. Caroff S., Mann S. Neuroleptic malignant syndrome. // Medical Clinics of North America. 1993; 77:185-202.
3. Levenson J. The neuroleptic malignant syndrome. // Am J Psychiat 1985; 142(10): 1137-45.
4. Yamawaki S., Yano E., Terakawa N. et al. On the results of a nationwide survey on neuroleptic malignant syndrome. // Hiroshima J Anesthesia 1988; 24(suppl): 52-67.
5. Caroff S Mann S., Lazarus A et al. Neuroleptic malignant syndrome: Diagnostic issues. // Psychiatric Annals. 1991; 21:130-47.
6. Deng M., Chen G., Phillips M. Neuroleptic malignant syndrome in 12 of 9,792 Chinese inpatients exposed to neuroleptics: A prospective study. // Am J Psychiatry 1990; 147:1149-55.
7. Keck P., Pope H., Cohen B. et al. Risk factors for neuroleptic malignant syndrome. // Arch Gen Psychiatry 1989; 46:914-8.
8. Lazarus A., Mann S., Caroff S. The neuroleptic Moligant syndrome and related conditions. // Washington, DC./American Psychiatry Press Inc. 1989.
9. Gelenberg A., Bellinghausen B., Wojcik J., et al. Patients with neuroleptic malignant syndrome histories: What happens when they are rehospitalized? // J Clin Psychiatry 1989; 50:178-80.
10. Gelenberg A. A prospective study of neuroleptic malignant syndrome in a short-term psychiatric hospital. // Am J Psychiatry 1988; 145:517-8.
11. Keck P., Pope H. G., Mc Elroy. Declining frequency of neuroleptic malignant syndrome in a hospital population. // Am J Psychiatry 1991; 148:880-2.
12. Caroff S., Mann S. Neuroleptic malignant syndrome. // Psychopharmacol Bull. 1988; 24:25-9.
13. Delay J., Deniker P. Drug-induced extrapyramidal syndromes. // Haudbook of clinical neurology. New York, 1968; 6:248-66.
14. Haberman M. Malignant hyperthermia. An allergic reaction to thioridazine therapy. // Arch intern Med 1978; 138:800-1.
15. Pope H., Cole J., Choras P., Fulwiler G. Apparent neuroleptic malignant syndrome with clozapine and litium. // J Nerv Ment Dis 1986; 174(8): 493-5.
16. Rosebush P., Stewart T. A Prospective analysis of 24 episodes of neuroleptic malignant syndrome. // Am J Psychiatry 1989; 146:717-25.
17. Malin D.I. Clinic and therapy of paroxysmal schizophrenia complicated by neuroleptic malignant syndrome. // Diss… cand. honey. Sciences. M. 1989; 185.
18. Malin D.I., Kozyrev V.N., Neduva A.A., Ravilov R.S. Malignant neuroleptic syndrome: diagnostic criteria and principles of therapy. Sots. and wedge. psychiatrist. 1997; 7(1): 76-81.
19. Tsygankov B.D. Clinical and pathogenetic regularities in the development of febrile attacks of schizophrenia and the system of their therapy. M.I.A. "Norma" 1997; 232.
20. Ravkin N.G., Golodets R.G., Samter N.F., Sokolova-Levkovich A.P. Life-threatening complications observed in patients with schizophrenia in the treatment of their neuroleptic drugs. // Question. psychonarcology M., 1967; 47-61.
21. Burke R., Fahn S., Weinberg H. et al. Neuroleptic malignant syndrome caused by dopamine-depleing drugs in a patients with Hungtiugton desease. // Neurology 1981; USI: 8.
22. Henderson V., Wooten G. Neuroleptic malignant syndrome: A pathogenic role for dopamine receptor blockade? // Neurology 1981; 31(2): 123-37.
23. Coons D., Hillman F., Marshall R. Treatment of NMS with dautrolene sodium: A case report. // Amer J Psychiat 1982; 138(7): 944-5.
24. Khan A., Jaffe J., Nelson W., Vorrison B. Resolution of neuroleptic malignant syndrome with dantrolene sodium. // J Clin Psychiat 1985; 46(6): 244-6.
25. May D., Morris S., Stewart R. et al. Neuroleptic malignant syndrome: response to dantrolen sodium. // Ann Intern Med 1983; 98(2): 183-4.
26. Renfordt E., Wardine B. Elektrokrumpf-und Dantrolen-Behandlung einer akuten febrilen Katatoni: Ein kasuistischer Beitrag. // Nervenarzt 1985; 56(3): 153-6.
27. Kekelidze Z.I., Chekhonin V.P. Critical states in psychiatry. M. 1997; 362.
28. Chekhonin V.P., Morozov T.V., Morkovkin V.M., Kekelidze Z.N. Immunochemical study of the permeability of the blood-brain barrier in critical conditions caused by febrile schizophrenia and acute alcoholic encephalopathies. Mat. 8th congress neuropathol. and a psychiatrist. // M. 1988; Z: 132-4.
29. Dhib-Jalbut S., Hesselbrock R., Mouradian M., Means E. Bromocriptine treatment of neuroleptic malignant syndrome. // J Clin. Psychiat 1987; 48(2): 69-73.
30. Sakkas P., Davis J., Janicak P. et al. Drug treatment of the neuroleptic malignant syndrome. // Psychopharmacol Bull 1991; 27:381-4.
31. Lazarus A. Treatment of neuroleptic malignant syndrome with electroconvulsive therapy. // J Nerv Ment Dis 1986; 174(1): 47-9.
32. Addonizio G., Susman V. ECT. As a treatment alternative for patients with symptoms of neuroleptic malignant syndrome. // Amer J Psychiat 1987; 48(1): 47-51.
33. Hermesh H., Aizenberg D., Weizman A. A successful electroconvulsive treatment of neuroleptic malignant syndrome. // Acts psychiat Scand 1987; 75(3): 287-9.
Human consciousness is an extremely complex matter and has not yet been fully studied. The brain diligently “bypasses” any irritating factors that can upset the state of a precarious balance and take us out of that small patriarchal world into which we have driven ourselves. So, we do not attach importance to the obvious signs of formidable diseases and ignore the insistent calls of doctors to come to grips with their own health, if only to delay the “exit” to the real world. For a week, for a day, for an hour... But if we are faced with what is considered a sentence in society, we give up without even thinking about the possibility of fighting fate. Why did we allow ourselves such a lyrical introduction, you ask? The fact is that the topic of our conversation today - neuroleptic malignant syndrome - is in a sense an indicator of human inertia and an extra confirmation that many things that surround us are not what they seem at first glance.
Imagine that you went to the doctor complaining of heart failure, high fever, and depressed mood. It would seem that the symptoms are “harmless” and not threatening with serious consequences. Therefore, having passed several tests, without any excitement, you expect the doctor to prescribe standard treatment. But when you are given a diagnosis of neuroleptic malignant syndrome, your mind picks out only the first word of everything that has been said, after which the world around you suddenly loses all its colors. “I have cancer, and I had so little time to do. I have a family, a child… I can no longer be with them.” Most ordinary people, far from medicine, will think something like this, and the brain will helpfully draw a black and white picture of the near future. Queues to the district oncologist, waiting for unbearable pain, formal help from colleagues, slow and painful extinction ... Meanwhile, neuroleptic syndrome (pay special attention to the absence of the prefix "malignant") has nothing to do with oncology.
This is a very rare, but extremely life-threatening condition, due in most cases to a pronounced side effect from taking certain psychotropic drugs. And it does not require self-pity or ever-increasing doses of painkillers, but emergency care. In other words, neuroleptic malignant syndrome is, in fact, acute poisoning. Therefore, if any clinical manifestations occur (we will consider the symptoms in detail in the appropriate section), you should immediately call an ambulance, and not look for a place in the cemetery. We assure you, you will still make it there. But if you act fast, not this time!
Risk factors and prevalence
1. Long-term use of antipsychotics (including atypical) of the following groups:
- butyrophenones (aromatic ketones): haloperidol, domperidone, benperidol;
- phenothiazines: dibenzothiazine, thiodiphenylamine, paradibenzothiazine;
- thioxanthenes: clopixol, truxal, fluanxol.
2. Side effects of antipsychotic treatment:

3. Features of the anamnesis
- electroconvulsive therapy without sufficient control of the patient's condition;
- significant dehydration of the body;
- physical or alimentary (caused by a deficiency of vitamins, proteins or iron) exhaustion;
- severe psychomotor agitation;
- catatonic syndrome;
- signs of chronic alcoholism (confusion, delirium, affective psychosis);
- water-electrolyte imbalance;
- thyroid dysfunction;
- intercurrent infection.
4. Organic brain damage due to ...
- ... craniocerebral injury;
- ... post-traumatic encephalopathy;
- ... persistent extrapyramidal disorder;
- ... dementia.
5. Other reasons
- high humidity and air temperature;
- male gender.
Patients of what age categories can be conditionally attributed to the risk group? There is no consensus on this issue among researchers. Some of them include the elderly (over 50 years). Others, on the contrary, cite data according to which the most “dangerous” age is from 20 to 40 years. Still others distinguish two risk groups: the first - 20-30 years old, the second - from 70 and older.
How common is neuroleptic malignant syndrome (NMS)? Most authors indicate that among patients treated with antipsychotics or highly potent antipsychotics, the incidence rate ranges from 0.02% to 3.23% (according to some sources - up to 12.2%). If the treatment was based on low-potency drugs, neuroleptic syndrome occurs somewhat less frequently (from 0.02% to 1.4%). It is also noted that the use of the latest pharmacological agents (released in the 1990s - 2000s) and the gradual abandonment of traditional drugs significantly reduces the likelihood of developing NMS (up to 0.01%).
Symptoms
 Remember, at the beginning of the article we tried to debunk the common misconception among the people, according to which neuroleptic malignant syndrome and cancer are identical concepts. And the symptoms of NMS are another confirmation of this. Most of them can hardly be called deadly, which does not mean that they can be fearlessly ignored. In addition, the neuroleptic syndrome in its acute phase worries the patient for no more than a month (most often from 7 to 14 days). But if the patient "missed" the initial manifestations of NMS, considering them insignificant, he may need emergency care and a long period of rehabilitation, which, under unfavorable circumstances, will take more than one week.
Remember, at the beginning of the article we tried to debunk the common misconception among the people, according to which neuroleptic malignant syndrome and cancer are identical concepts. And the symptoms of NMS are another confirmation of this. Most of them can hardly be called deadly, which does not mean that they can be fearlessly ignored. In addition, the neuroleptic syndrome in its acute phase worries the patient for no more than a month (most often from 7 to 14 days). But if the patient "missed" the initial manifestations of NMS, considering them insignificant, he may need emergency care and a long period of rehabilitation, which, under unfavorable circumstances, will take more than one week.
1. Progressive muscle weakness. It occurs in 97% of patients and is most often accompanied by fever. The severity of clinical manifestations can be different: from "harmless" increased muscle tone to the symptom of "lead pipe" (extreme resistance to passive movements).
2. Extrapyramidal disorders
- bradykinesia and akinesia;
- symptom of "gear wheel";
- myoclonus;
- chorea;
- dysarthria;
- dysphagia;
- signs of dystonia (tonic spasm of masticatory muscles, oculogyric crisis, blepharospasm);
- hyperreflexia;
- opsoclonus and nystagmus;
- tremor;
- opisthotonus;
- aphonia;
- akathisia;
- epileptiform seizures;
- discoordination;
- difficulty walking.
3. A strong increase in body temperature, sometimes up to 41-42 degrees (the patient needs immediate help). In rare cases, neuroleptic malignant syndrome develops against the background of normal (36.5-37 degrees) indicators.
4. Numerous somatic disorders
- cardiac dysrhythmia (most often tachycardia);
- sharp fluctuations (lability) of blood pressure;
- blanching of the skin;
- increased salivation;
- tachypnea;
- severe sweating;
- urinary incontinence.
5. Signs of dehydration

6. Mental disorder
- persistent feeling of anxiety;
- confusion of thoughts;
- delirium;
- severe catatonia;
- akinetic mutism;
- amental or oneiric clouding of consciousness;
- in some cases - coma.
Diagnostics
1. The most informative laboratory tests
- general blood analysis;
- clinical analysis of urine;
- group of liver tests;
- analysis of the gas composition of arterial blood;
- toxicological screening (urine and serum);
- study of cerebrospinal fluid obtained by lumbar puncture;
- prothrombin time.
2. Instrumental research
- chest x-ray;
- EEG (electroencephalography).
3. Key laboratory findings that may confirm the diagnosis of NMS
- severe leukocytosis (noted in 98% of patients) or a significant shift to the left of the leukocyte count (in 40% of cases);
- elevated levels of creatine phosphokinase (97-99% of patients). If NMS is caused by taking antipsychotic drugs, such indicators occur in 70% of patients;
- metabolic acidosis (70-75%).
4. Factors that may indicate NMS
- electrolyte imbalances (hypo- or hypernatremia, decreased levels of calcium, potassium, magnesium);
- an increase in the concentration of alanine aminotransferase, aspartate aminotransferase, aldolase, lactate dehydrogenase or lactic acid;
- decrease in the level of serum iron;
- coagulopathy;
- myoglobinuria and azotemia.
Differential Diagnosis
 NMS should be distinguished from some pathological conditions that have similar clinical manifestations, but different treatment from neuroleptic syndrome:
NMS should be distinguished from some pathological conditions that have similar clinical manifestations, but different treatment from neuroleptic syndrome:
- serotonin syndrome;
- lethal catatonia;
- some infectious diseases (encephalitis, tetanus, meningitis, rabies, sepsis);
- epileptic status;
- withdrawal states (a consequence of the withdrawal of alcohol, barbiturates or sedatives);
- ischemic stroke;
- malignant hyperthermia;
- heatstroke;
- severe forms of dystonia;
- poisoning with drugs and chemical compounds (amphetamine, salicylates, salts of heavy metals, organophosphorus compounds, anticholinergics, strychnine, lithium);
- autoimmune disorders;
- tumors of the central nervous system.
Possible Complications
- rhabdomyolysis;
- dangerous pathologies of the respiratory system: respiratory distress syndrome, pulmonary embolism, aspiration pneumonia, pulmonary edema;
- epilepsy;
- infectious pathologies: sepsis, colibacillary fasciitis, urinary tract lesions);
- neuronal cerebral degeneration;
- acute liver failure;
- pathologies of the cardiovascular system: myocardial infarction, arrhythmia, sudden cardiac arrest;
- DIC syndrome.
Treatment
Effective therapy for NMS is possible only in a specialized hospital (intensive care unit or intensive care unit), although the first emergency aid can be provided immediately. The treatment itself usually includes the following activities:
1. Immediate cancellation of any antipsychotics or potent drugs.
2. Restorative therapy (if emergency care is no longer required):
- normalization of body temperature;
- prevention of thrombosis;
- hydration;
- removal of muscle rigidity;
- aspiration prevention;
- therapeutic massage sessions;
- physiotherapy of the chest organs;
- complete nutrition.
3.  Drug therapy
Drug therapy
- intravenous administration of sodium nitroprusside (bicarbonate);
- antihypertensive drugs: oxygen, nifedipine;
- antipyretics;
- carbidopa and levodopa (fighting fever);
- muscle relaxants;
- amantadine, bromocriptine, dantrolene (direct therapy for NMS);
- lorazepam and diazepam (severe catatonia);
- iron preparations.
4. Auxiliary manipulations (help in case of complications)
- installation of a urinary catheter;
- artificial ventilation of the lungs and intubation (for serious breathing problems);
- use of a nasogastric tube;
- hemodialysis (if there are signs of renal failure);
5. Electroconvulsive therapy is indicated for confusion, high temperature, profuse sweating and obvious catatonic symptoms (6 to 10 sessions).